By Shantell M. Kirkendoll
Duke University researchers created a computer program that determines, with 94% accuracy, if a person's age-related macular degeneration will worsen within a year.
The deep learning algorithm, featured in an Oct. 19 study in JAMA Ophthalmology, analyzes detailed eye scans to predict if the common eye condition will progress to a more severe stage known as geographic atrophy (GA).
This faster foresight could streamline clinical trial recruitment and aid rollout of targeted treatments designed to preserve the vision of older adults.
“Being able to predict disease progression means we can be proactive, potentially halting its progression and improving patient outcomes,” said senior study author Eleonora Lad, MD, PhD, director of clinical research and associate professor at the Duke Eye Center.
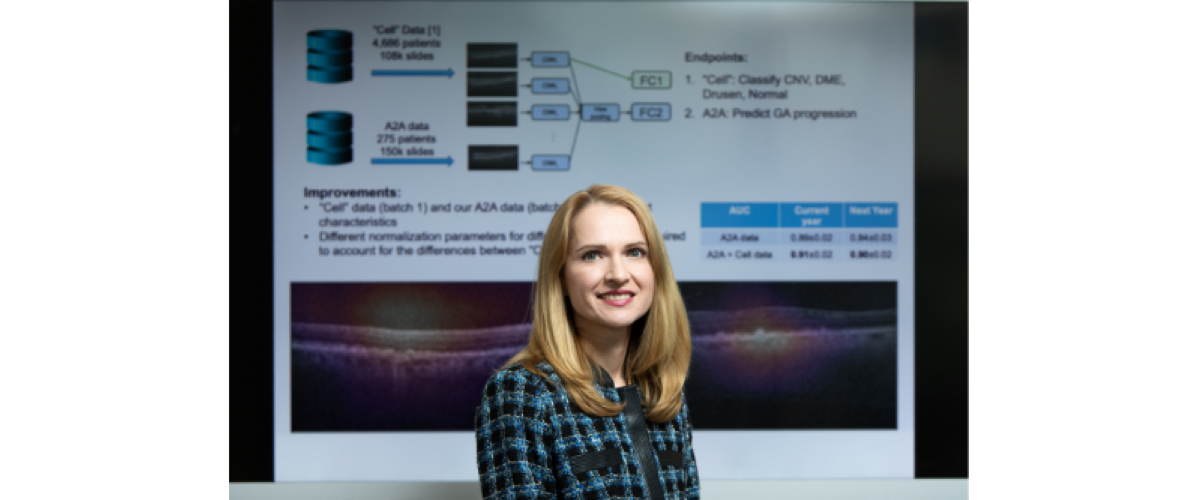
Eye doctors at Duke Eye Center collaborated with Duke AI Health, the Duke Department of Electrical and Computer Engineering and global experts on the recent study of the algorithm known as DeepGAze.
"This predictive tool could transform how we screen for the disease, how often we see patients, and even when to start treatments,” Lad said.
Progression from intermediate AMD to geographic atrophy represents a transition from a largely asymptomatic condition to one that may devastate central vision, which is needed to read, drive and see pictures and faces.
The U.S. Food and Drug Administration recently approved medications that can offer a reprieve for the 1.5 million Americans diagnosed with geography atrophy. Izervay can slow GA’s progression and Ladd led clinical trials for Pegcetacoplan, the first FDA-approved medication for GA.
The Lancet recently highlighted Phase 3 clinical trial results confirming the ability of Pegcetacoplan to curb GA lesion growth with monthly or bimonthly injections.
Algorithms like DeepGAze, like other technology used to track diabetic retinopathy, are poised to refine the diagnostic process and help doctors figure out who’ll benefit most from maintenance and treatment.
In JAMA Ophthalmology, researchers detail how the DeepGAze algorithm sorted through volumes of spectral-domain optical coherence tomography scans of the retina to spot which eyes would progress from intermediate stage AMD to geographic atrophy within a year.
The program used data from several U.S. centers and the Age-Related Eye Disease Study (AREDS2). In all, 417 patients were involved in the study. The ability of DeepGaze to predict progression to GA within a year had a true positive rate of .94. In other words, it was right 94% of the time.
Even when experts added annotations, a time-consuming and expensive task, to the model, it didn’t get significantly better than when it was working on its own.
Additional Authors: Co-first authors, Eliot R. Dow, MD, PhD and Hyeon Ki Jeong, PhD; Ella Arnon Katz, MD; Cynthia A. Toth, MD; Dong Wang, PhD; Terry Lee, MD; David Kuo, MD; Michael J. Allingham, MD, PhD;
Majda Hadziahmetovic, MD; Priyatham S. Mettu, MD, PhD; Stefanie Schuman, MD; Lawrence Carin, PhD; Pearse A. Keane, MD; and Ricardo Henao, PhD.
Funding: National Eye Institute (K23EY026988) and the Veteran’s Affairs Health System (I01 CX002116). The AREDS2 trial was supported by the National Eye Institute (1R01EY023039).
Disclosure: Lad works as a consultant for Apellis, which makes Pegcetacoplan