Severe Vitamin A Deficiency and Xerophthalmia Leading to Corneal Perforation
Authors
Riya Shah BS, Jae Kim MD, Joshua Barbosa MD, Patrick SY Lee MD PhD, Mark McDermott MD*
Introduction
Nutritional deficiencies have been recognized as significant contributors to various systemic and ocular disorders. Among these deficiencies, vitamin A plays a crucial role in maintaining ocular health. Vitamin A deficiency is extremely rare in the United States, affecting about 0.3% of the general population.1 Etiologies include insufficient nutritional uptake or malabsorptive co-morbidities such as inflammatory bowel disease, cirrhosis, pancreatic insufficiency, or pregnancy.2Severe vitamin A deficiency can lead to xerophthalmia, conjunctival xerosis, corneal ulceration, and xerophthalmic fundus. This case presentation follows a patient with long-standing cirrhosis found to have ocular manifestations of nutritional vitamin A deficiency, eventually necessitating penetrating keratoplasty (PK) secondary to corneal perforation.
Case Report
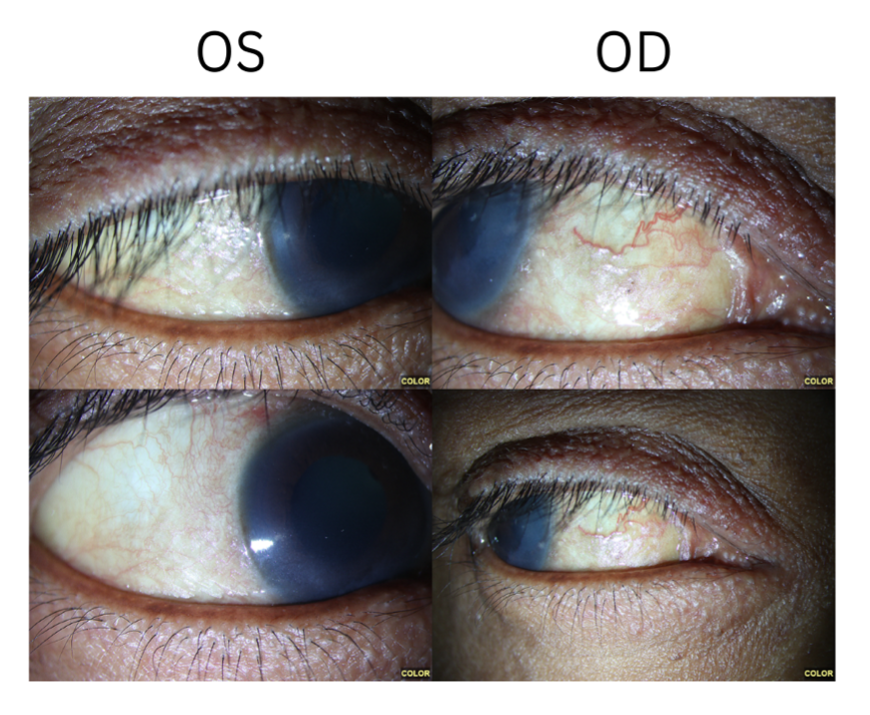
A 42-year-old woman with a past medical history of gastroesophageal reflux disease and alcoholic cirrhosis presented with chronic bilateral blurry vision in the absence of trauma. The patient endorsed a 10-pack-year smoking history and long-standing alcohol use since the age of 17. Her diet was poor as she had limited time to eat at work, and the patient had pre-packaged lunch snacks (nutritionally deficient snack consisting of meat, cheese, and crackers) in her hand while in the clinic, which she stated was a normal meal for her. The patient appeared underweight and emaciated on presentation. On initial examination, she had a visual acuity of 20/100 in the right eye and Counting Fingers at 4 feet in the left eye, without improvement on pinhole. Intraocular pressures were 16 in the right eye and 18 in the left eye, with sluggish pupil reactions bilaterally but no afferent pupillary defect. Slit lamp examination revealed diffuse xerosis of the conjunctiva and punctate epithelial erosions approaching confluency in both eyes (Figure 1). Posterior exam showed no apparent abnormalities, with a cup-to-disc ratio of 0.3 but no optic nerve pallor in either eye. Optical coherence tomography (OCT) imaging showed diffuse thinning of ganglion cell layer bilaterally, out of proportion to retinal nerve fiber layer thinning, consistent with a nutritional or toxic optic neuropathy. Full-field electroretinography (ERG) showed undetectable signal (“flat ERG”) on rod response and dark-adapted response, consistent with vitamin A deficiency. Goldmann visual field testing showed significant field constriction bilaterally. Nutritional labs showed malnutrition, including a vitamin A level of 8.9 ug/dl (normal: 30-60 ug/dl). Complete blood count revealed a hemoglobin of 8.5 with a platelet count of 94,000. Daily oral vitamin A 10,000 unit capsules were started, as well as a multivitamin and topical artificial tears. The patient also expressed frustration with her history of alcohol use, and a social work referral as well as other resources were provided. Plans for close follow-up were made.
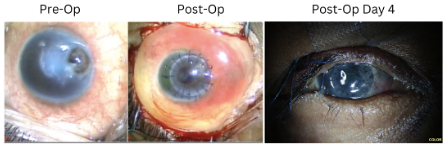
Approximately 2 weeks later, the patient presented to an outside hospital with a 4 mm temporal corneal perforation in the right eye that she noted after applying artificial eyelashes. The patient experienced a decline in visual acuity to light perception only vision in the right eye. She was seen by the ophthalmology service at her local hospital and the area of perforation was temporarily glued with instructions to follow-up at our clinic the next day. Penetrating keratoplasty was performed the same day along with a temporary tarsorrhaphy to aid in epithelial healing (Figure 2). Further pathological examination of the host cornea showed keratitis and neovascularization consistent with the diagnosis of severe vitamin A deficiency along with xerosis. On postoperative day 4, the patient's right eye visual acuity had improved to 20/400, and intraocular pressure was 20. Oral prednisone, topical brimonidine, topical prednisolone acetate 1%, and moxifloxacin drops were started with plans for continued follow-up.
Discussion
Vitamin A is a fat-soluble vitamin with essential functions in visual pigment regeneration, immune system strength, and mucous membrane maintenance. While the occurrence of vitamin A deficiency is uncommon in developed regions, deficiency of this vitamin can lead to night blindness, corneal thinning, and conjunctival metaplasia.3 The patient's alcoholism and poor nutritional intake along with the laboratory findings showing vitamin A deficiency point towards the potential etiology of her visual symptoms.
Vitamin A plays a critical role in maintaining ocular health. In addition to its well-known role in the visual cycle of rhodopsin, it also regulates multiple genes through its binding of nuclear retinoic acid receptors. At the ocular surface, vitamin A is necessary for differentiation of non-squamous epithelium, and regulates the metabolism of corneal epithelial cells.2 As a result, its deficiency induces metaplasia and keratinization of the epithelium, with loss of differentiation into goblet cells. Clinically, the conjunctiva becomes wrinkled, with the appearance of Bitot spots. The cornea initially demonstrates punctate keratopathy, which further progresses to keratinization. Ulceration may then occur with detachment of this keratinized layer, while keratomalacia and stromal melt results from severe stromal necrosis, with resulting descemetocele or corneal perforation as seen in our case.3
Treatment consists of supplementation of vitamin A, which is highly effective, even for more severe presentations such as ulcerations and liquefactive necrosis. However, caution is warranted towards repletion, as hypervitaminosis A has been linked to liver toxicity and elevated intracranial pressure with papilledema.4
Corneal perforation is the most feared end-stage result of xerophthalmia, often requiring penetrating keratoplasty. In cases of penetrating keratoplasty performed for corneal perforation, the success rate varies, ranging from 50-80%,5 with recovery occurring over the next 3-4 months. This patient showed promising success as her visual acuity was beginning to improve on postoperative day 4.
Conclusion
This case emphasizes the critical importance of recognizing and addressing severe vitamin A deficiency in patients with characteristic signs and symptoms, underlining the need for prompt intervention to mitigate potential complications, including corneal perforation.
References
- Pfeiffer CM, Sternberg MR, Schleicher RL, et al. The CDC's Second National Report on Biochemical Indicators of Diet and Nutrition in the U.S. Population is a valuable tool for researchers and policy makers. J Nutr 2013; 143: 938S-947S. 2013/04/19. DOI: 10.3945/jn.112.172858.
- Sommer A, Green WR and Kenyon KR. Clinicohistopathologic correlations in xerophthalmic ulceration and necrosis. Arch Ophthalmol 1982; 100: 953-963. 1982/06/01. DOI: 10.1001/archopht.1982.01030030961014.
- Sommer A. Effects of vitamin A deficiency on the ocular surface. Ophthalmology 1983; 90: 592-600. 1983/06/01. DOI: 10.1016/s0161-6420(83)34512-7.
- Velasco Cruz AA, Attie-Castro FA, Fernandes SL, et al. Adult blindness secondary to vitamin A deficiency associated with an eating disorder. Nutrition 2005; 21: 630-633. 2005/04/27. DOI: 10.1016/j.nut.2004.12.003.
- Gurnani B and Kaur K. Penetrating Keratoplasty. StatPearls. Treasure Island (FL) ineligible companies. Disclosure: Kirandeep Kaur declares no relevant financial relationships with ineligible companies., 2023.
Statement of Ethics
Written informed consent for patient information and images to be published was provided.
Conflict of Interest Statement
All authors of this work have no financial disclosures.
Funding
This work was supported by Research to Prevent Blindness [P30-EY04068] (Non restricted grant to the Department of Ophthalmology, Visual and Anatomical Sciences).