Artificial Intelligence is Shaping the Future of Eye Care – And Duke is Leading the Way
Artificial intelligence (AI) leverages the growing power and speed of computers to solve complex problems. AI is transforming medical research and clinical practice – and ophthalmology is leading the way.
“One of the most successful ways that AI has been applied recently is in the area of ‘computer vision,’ which is the assessment and interpretation of images,” explains Felipe Medeiros, MD, PhD, Joseph A.C. Wadsworth Professor of Ophthalmology. “We can apply sophisticated AI algorithms, such as ‘deep learning’ neural networks, which are capable of very complex pattern recognition tasks, to identify whether specific characteristics are present in an image or not.
“In ophthalmology we have a wealth of eye images – fundus photographs, optical coherence tomography (OCT), etc. – that are fundamental to the diagnosis, monitoring, and treatment of a number of eye diseases, so this field is ideally suited for deep learning applications,” says Medeiros, who is Duke Ophthalmology’s vice chair of technology and leads the clinical research unit. “The development of such applications has been increasing at an astounding rate. In several disciplines, including ophthalmology, researchers have proven that deep learning algorithms can actually outperform humans in some tasks.”
Minimizing mistakes, maximizing efficiency
Deep learning algorithms not only reduce labor and equipment costs but can also eliminate errors that occur from the subjective interpretation of diagnostic images by humans. They can also bring screening and diagnosis to underserved areas where specialists may be limited.
“There will always be a significant role for human contribution and physicians’ expertise, so there is no need to worry about a future in which patients are treated entirely by computers,” assures Eleonora Lad, MD, PhD, an associate professor of ophthalmology and clinician-scientist who is researching applications of AI to improve diagnosis and treatment of age-related macular degeneration. “Physicians have limited time and bandwidth. Machine learning can provide us with new information, faster, so we can make more informed diagnoses and spend more time working with our patients on the best treatment plan.”
Duke Ophthalmology at the forefront
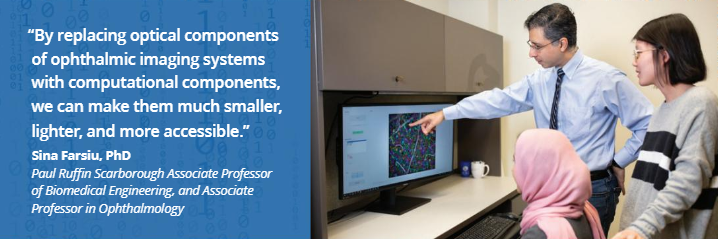
Duke Ophthalmology has a long track record of developing AI technology to improve eye care. Sina Farsiu, PhD, who holds joint appointments in the Pratt School of Engineering and the Department of Ophthalmology, is a pioneer in the use of AI in ophthalmology. He established the Vision and Image Processing Laboratory at Duke Eye Center a decade ago and has developed numerous ophthalmic image analysis tools that are freely shared online and used in multicenter clinical trials around the world.
Duke University is also finding innovative ways to apply AI to a range of disciplines. In 2019, Duke appointed Lawrence Carin, PhD, one of the world’s leading experts on machine learning and artificial intelligence, as vice president of research. Duke Ophthalmology looks forward to collaborating with the AI Health Data Science Initiative, leveraging the university’s focus on artificial intelligence and its culture of multidisciplinary collaboration.
“Larry’s team members are experts in computer science; we have the top minds in ophthalmology,” Medeiros says. “We bring them clinical challenges, and they bring us innovative ways of creating algorithms to solve them. Together, it’s a great fit that would be hard to find anywhere else.”
Carin agrees. “Duke Ophthalmology is very well positioned in this space, as it already has multiple clinician-scientists who recognize the opportunity and are engaged in leading research. Duke is also the home of leadership in the fundamentals of AI. By bringing Duke Ophthalmology and the broader Duke methodological AI leaders together, Duke is positioned to be a global leader on the application of AI to the transformation of ophthalmological care.”
Duke Ophthalmology is applying AI to advance research and improve treatment for several common and important eye diseases. Some examples:
Glaucoma
Glaucoma is a leading cause of irreversible blindness in the world. Because the disease remains largely asymptomatic until late stages, there is a great need to develop affordable approaches for screening before visual impairment occurs – when early intervention can still save sight.
Medeiros’s research team has developed several AI algorithms that promise to detect glaucoma more quickly and efficiently. One algorithm has been proven to accurately quantify the amount of damage a patient has in the optic nerve from just a fundus photograph, and tell us whether the patient is likely to have glaucoma or not.i Using the power of AI, researchers were able to closely replicate OCT estimates of neural loss. The method also removed subjectivity, and even outperformed human specialists in the interpretation of fundus photographs for glaucoma.ii And, because photographs are less expensive and more widely available than OCT, this method offers the potential to bring improved screening and diagnosis to underserved locations.
Age-Related Macular Degeneration
Once age-related macular degeneration (AMD) progresses to its late stages, there is no treatment for 85% of cases with the dry form (geographic atrophy), and loss of central vision is inevitable. Lad is on a mission to find biomarkers that predict disease progression, both to better understand the genesis and progression of disease and to test potential treatments on patients before vision loss becomes irreversible. AI is helping to speed that search.
“The National Eye Institute’s multicenter, prospective, Age-Related Eye Disease Study 2 (AREDS2) is providing a true goldmine of data on aging and AMD, including several types of high-resolution retinal images and demographic, functional, and genetic data from study participants over several years. We are collaborating with Larry Carin’s team to mine the retinal images from this study and to develop deep learning algorithms to uncover biomarkers that indicate rapid disease progression,” Lad says.
“It took years and much grant funding for research associates in Dr. Cynthia Toth’s lab to grade every OCT image from the study and develop a true encyclopedia of annotated OCT features that predict disease progression,” she notes. “Using deep learning/AI, we hope to do this much more quickly and inexpensively, so we can predict which patients would progress to vision loss over a timeframe as short as 1-2 years and can enroll them into promising clinical trials.”
Already, the team has created an algorithm capable of grading three-dimensional OCT images with 91% accuracy at predicting which patients will develop geographic atrophy within one year.
“After these algorithms are refined and validated, they can be incorporated into OCT machines,” Lad says. “Then, ophthalmologists and optometrists could screen their patients during routine exams, determine their risk of progression to advanced disease (neovascular or dry), and refer them to a retinal specialist.”
Diabetic Retinopathy
Farsiu, together with Duke Ophthalmology clinician-scientists Scott Cousins, MD, and Prithu Mettu, MD, developed the first algorithm that could distinguish AMD and diabetic retinopathy from each other, and from normal eyes, using OCT images.iii This was the first algorithm with the ability to process images from different centers with different imaging protocols.
Farsiu’s postdoctoral mentee, Reza Rasti, PhD, in collaboration with Michael Allingham, MD, PhD, Cousins, and Mettu, is now using AI to identify which diabetic retinopathy patients will respond best to anti-VEGF injections – before treatment starts. That means patients who would not respond well won’t have to go through this vision-saving, but complicated and expensive, treatment.
Imaging Technology
AI’s computational techniques also enable Duke researchers to develop more elegant imaging modalities, notes Farsiu, whose Vision and Image Processing Laboratory was the first to develop a fully automatic deep learning algorithm that successfully uses clinical-grade OCT images of the retina to detect multiple diseases of the eye.
“By replacing optical components of ophthalmic imaging systems with computational components, we can make them much smaller, lighter, and more accessible,” he says. “For example, in collaboration with Joseph Izatt, PhD, we have been able to shrink an adaptive optics scanning laser ophthalmoscope from a desktop size down to a portable handheld unit, which allows us to use this tool on infants and children, who have a hard time sitting still in front of a traditional unit.”
Data Analysis for Clinical Trials
Farsiu’s lab is also collaborating with Duke retinal specialist Glenn Jaffe, MD, to use AI to rapidly analyze data in multicenter international clinical trials for new therapies for blinding diseases. In one study, Farsiu’s PhD student, Jessica Loo, developed a fully automatic algorithm that could replicate the result of the clinical trial without any human involvement. This is a transformative change from the standard method of data analysis, which requires a human expert to review a computer’s analysis of each image to correct its mistakes – a time-consuming and expensive task.
“These are preliminary results, which we will need to replicate in other clinical studies,” Farsiu notes. “But if we can successfully conduct the data analysis for an entire clinical trial fully automatically without human involvement, and get the same results, that would significantly reduce the cost of trials, eliminate human error, and get promising treatments to patients faster.”
The U.S. Food & Drug Administration, the agency within the U.S. Department of Health and Human Services that assures the safety and effectiveness of drugs and medical devices in clinical trials, also recognizes the power and promise of AI. The FDA has recently organized an Ophthalmic Imaging Collaborative Community group as a strategic priority for the agency. Lad is a key member of this effort, whose goal is to develop guidelines for the use of AI technologies in the diagnosis and treatment of patients with eye diseases.
The ultimate goal, Medeiros notes, is to apply AI to clinical practice in ways that can improve patient care and satisfaction. That requires many stages and very diverse expertise. “First, we need to develop ideas to address clinically relevant questions. Then we need to gather the relevant data, build, refine, and validate the AI algorithms. And ultimately, we need to integrate those algorithms into clinical practice and prove that they lead to better patient outcomes.”
The department envisions developing a comprehensive Center for Artificial Intelligence in Ophthalmology at Duke integrated with the university’s AI research enterprise, that would unite clinician-scientists, engineers, data scientists, and health outcomes researchers, with the goal of supporting AI initiatives through each stage, from idea through implementation. The center would also help researchers mine the vast amount of data and images stored within the Duke Eye Center’s electronic health records system.
Increasingly, health care providers and researchers are seeing the opportunities that AI can open up. “Momentum is building,” Medeiros says. “This is a transformational moment in health care, and for all of us who are involved in patient care, artificial intelligence will help us do better medicine.”