
Training Inventors
Training programs at Duke Ophthalmology are focused on fostering education of the next generation of clinician-scientists and researchers. An important priority is encouraging innovation for trainees who have a curious mindset and strive for generating new ideas and problem solving.
With an emphasis on research, Duke Ophthalmology has created an environment where trainees feel comfortable generating new ideas and testing them through exploration and experimentation. Trainees are given space to explore their ideas and work with faculty mentors who provide guidance on the approach to innovation, including research and developing ideas into reality.
Once the research is completed and the innovation has been proven to make an impact on the field, the trainee and their mentor will work with the Duke Office for Translation and Commercialization (OTC), which offers expertise in turning translational research into fully realized products and services. OTC staff educate and guide the next steps of the tech transfer to bring the idea to the market. They help with patent applications, connections with industry partners, pharmaceutical, and medical device companies that want to invest in the ideas.
Duke Trainee Turned Inventor Gives Glaucoma Care an Upgrade
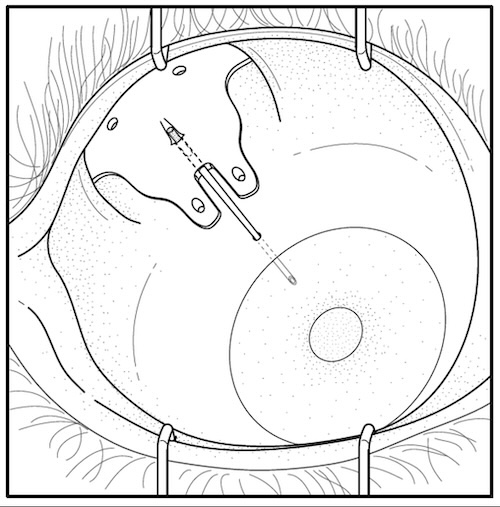
Rami Gabriel, MD was a resident at Duke Eye Center when he recognized a problem with eye drop adherence and administration following glaucoma drainage device (GDD) surgery. That’s when an idea began to form. Gabriel, now a Cornea Fellow in Duke Ophthalmology, is devising an improved GDD to reduce or eliminate post operative eye drops, reduce surgery difficulty, and ultimately tackle the primary goal of treating glaucoma: preventing blindness.
When medicated eye drops are too burdensome, surgeries can fail, and glaucoma can take a greater toll on a patient’s vision. But Gabriel has an elegant, yet simple, idea to help surgeries and patients succeed - what if the implant itself released critical glaucoma medicine into the eye that could relieve patients of ocular pressure and the pressure of applying eye drops post-surgery.
Central to Gabriel’s concept is a hydrogel, a unique, dissolvable polymer loaded with the glaucoma drugs that slowly release into the eye over time.
Time in the OR Leads to Enhanced Device
Beyond reduced patient burden, Gabriel sought to improve glaucoma treatment for surgeons as well. As a resident, Gabriel’s job in the operating room was to prepare the tube component of the GDD as the chief ophthalmologist, glaucoma specialist, and mentor, Leon W. Herndon Jr., MD, conducted the surgery. Herndon made the incision in the muscle of the eye and slipped the plate that would catch excess aqueous humor, the fluid built up from glaucoma, as Gabriel delicately tied off the tube at a separate station. In many practices, the primary surgeon performs Gabriel’s step after they implant the tube in the patient’s eye. This step requires finesse and can be cumbersome or lead to delays in surgery.
“Tying off all these tubes for the surgery,” Gabriel says, “I was like, ‘Well, maybe there’s a better way to do this. Maybe there’s a better way to do this for the patient too.’” That’s why his improved GDD design eliminated the tricky step of tying off the tube.
Gabriel soon found that the Duke Eye Center not only encouraged excellence in clinical practice, but it also emphasized mentorship, research, and innovation –– all features he credits as vital for finding a solution to a problem in glaucoma care.
When Duke trainees like Gabriel identify an unmet need in clinical practice, they can tap into Duke’s broad research capabilities to find a way to make an impact. So, when Gabriel had an idea to improve GDDs, he had an entire network ready to help him turn his idea into an invention.
Gabriel connected with Herndon and Pratap Challa, MD, both professors of ophthalmology and experts in glaucoma. Challa studies the cellular and genetic foundations of multiple glaucoma conditions as well as applications in glaucoma treatment like drug delivery and therapeutics. Challa, also the Duke Ophthalmology residency director, mentored Gabriel through the stages of translation research and is considered a co-inventor on Gabriel’s device.
Turning Ideas into Reality
With the support of his mentors and Duke’s innovation infrastructure, Duke Office of Innovation and Translation (OTC), Gabriel was able to devise a new device that eliminates a key barrier for patients –– eye drop burden –– and improves surgeries for practitioners. And like many innovative clinicians at Duke Eye Center, Gabriel’s inspiration was borne out of caring for his patients. As he continues to work with OTC on his drug-eluting GDD, he and his fellow clinicians at the Duke Eye Center continue to pursue novel translational ideas that can improve clinical practice at Duke and patient care everywhere. And as more funding organizations see the potential in young innovators like Gabriel or seasoned inventors like Challa, their impact on patients promises to grow.
“I've been very lucky to have some amazing mentors,” says Gabriel of Herndon and Challa. “Dr. Challa, who's my main mentor, has been teaching glaucoma for over 20 years, and it's one of the most prestigious programs to learn glaucoma from.”