Highlights from research, education and clinical care missions that drive advancements in ophthalmology.

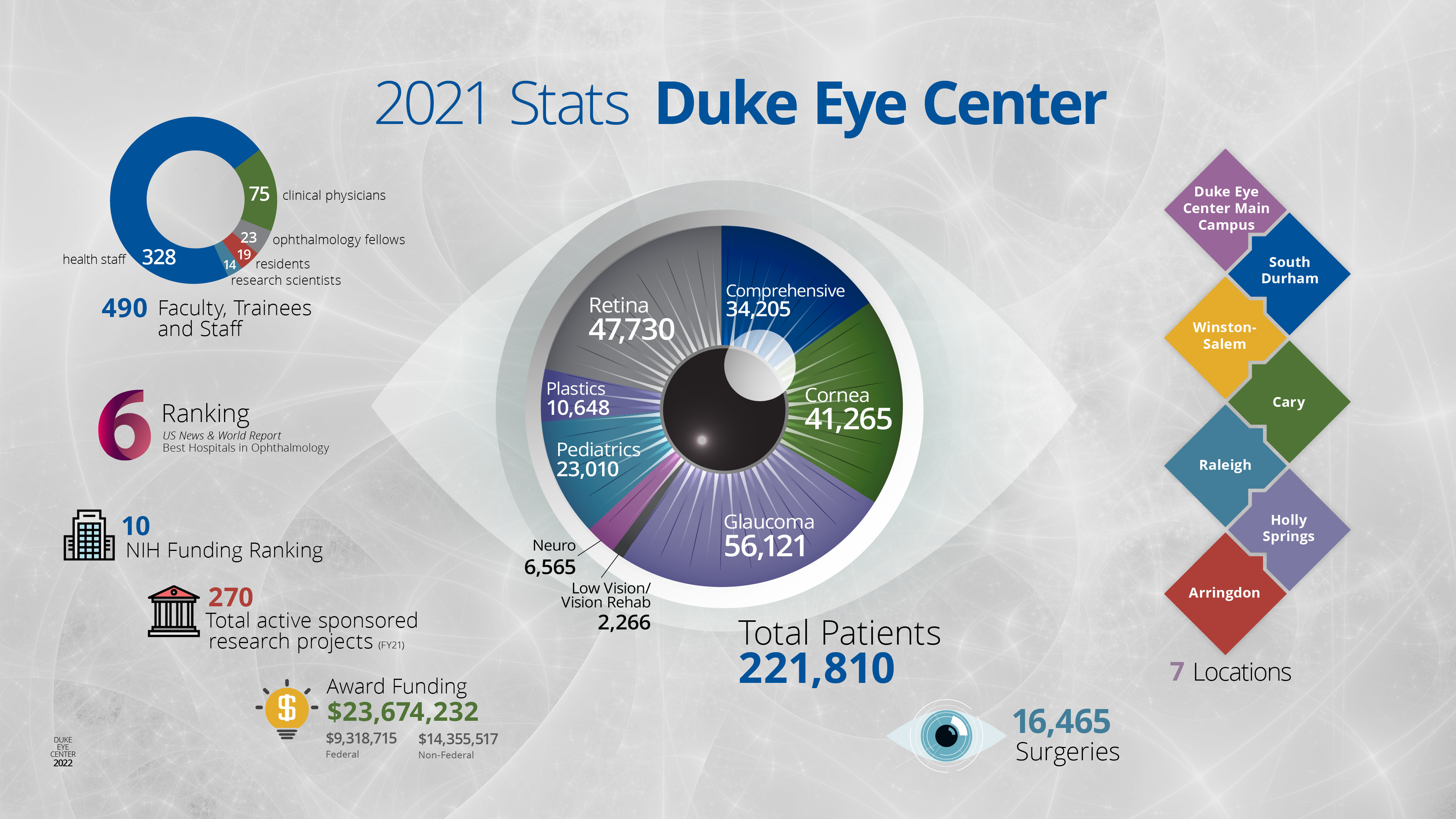
As a trailblazing leader in the field of ophthalmology, Duke Eye Center has taken a fully integrated approach to the key missions of research, education, and clinical care—endeavors dedicated to fulfilling our purpose of curing eye disease worldwide. The reputation of Duke Eye Center is further exemplified by being ranked as a top 10 ophthalmology hospital by the U.S. News and World Report annual best hospital rankings for more than 30 years.
Despite major setbacks due to the unrelenting COVID-19 pandemic, we are resolute in a proactive approach to make a difference in the lives of our patients, provide outstanding education for our trainees and colleagues, and pioneer research that revolutionizes the field of ophthalmology. Our people are at the center of our success and patients are at the center of everything we do. This issue of VISION demonstrates our newest contributions and impact on the field.
- The Duke Ophthalmic Registry, what is believed to be the nation’s largest single-institution multimodal database of ophthalmic records.
- Our Duke Global Ophthalmology Program relaunch aims to make an impact on international eye care.
- Improved Remote Diagnosis will allow easier access to care for patients at risk for severe eye disease.
- The new Duke Eye Stroke Clinic is a multidisciplinary approach for people affected by ischemic eye conditions.
- The new Research Roundup section in VISION provides a glimpse of important research contributions of our faculty and trainees.
- We have a great lineup of outstanding educational programs planned for 2022, including a new cornea fellows course.
The intentional integration of all three missions—research, education, and clinical care—these three vectors, led by our people, all moving together that has created a community of excellence that we are proud to call Duke Ophthalmology!
Sincerely,
Edward G. Buckley, MD
Vice Dean for Education, School of Medicine Chair, Department of Ophthalmology Vice Chancellor for Duke-National University Singapore Affairs Gills Professor of Ophthalmology Professor of Pediatrics Duke University School of Medicine
One-of-a-kind database created at Duke helps researchers to conduct large-scale, complex diagnostic studies using artificial intelligence (AI) and deep learning models
When asked what inspired him to develop the Duke Ophthalmic Registry—what is believed to be the nation’s largest single-institution multimodal database of ophthalmic records—Felipe Medeiros, MD, PhD, responded by simply saying, “meaningful research requires big data.”

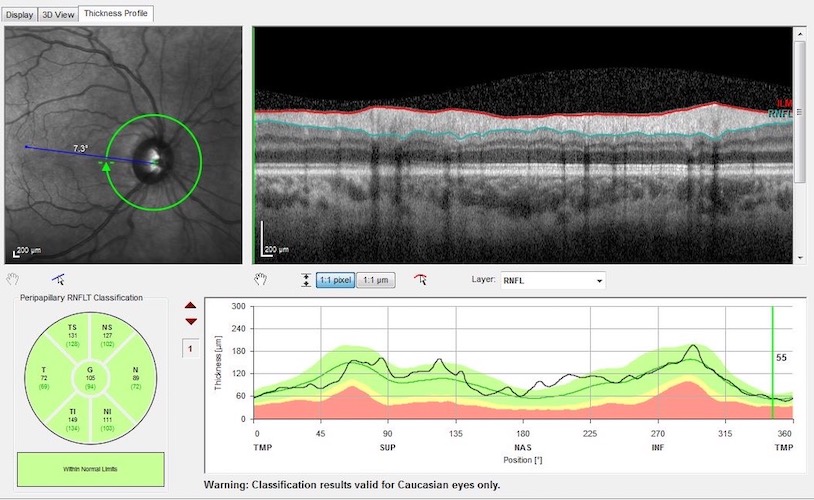
Medeiros, Joseph A.C. Wadsworth Professor of Ophthalmology, and one of the Top 5 Glaucoma Researchers in the World according to the Annals of Library and Information Studies, along with research scientist, Alessandro Jammal, MD, PhD, have spent the last four years building the database.
To complete the task, the team took on the Herculean effort of collecting and organizing the data from multiple sources including MaestroCare, Duke’s unified electronic medical record and clinical care application, images from Duke’s network of Optical Coherence Tomography (OCT) machines and the raw data stored in the Humphrey Field Analyzers and other machines. The result is a comprehensive, one-of-a-kind database that consists of clinical data and imaging which enables researchers to conduct large-scale, complex diagnostic studies using artificial intelligence (AI) and deep learning models.
However, Medeiros’ team did not stop there, they have also linked the imaging and functional data to patient visits at other clinics in the Duke Health System. This has allowed them to complete a broad range of studies. For example, they have been able to investigate blood pressure control based on more than 157,000 clinical visits and have linked this to the progression of glaucoma in certain patients.1

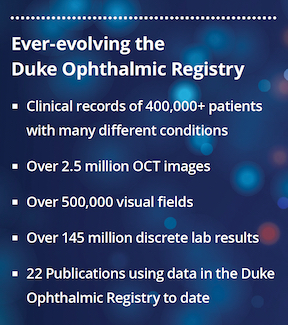
While the Registry was developed in Medeiros’ lab for the purpose of advancing glaucoma research, and it has been instrumental in helping to gain a greater understanding of the risk factors and prognosis for glaucoma among large populations, it also offers the opportunity to perform work on other fields such as the outcomes and treatments of macular degeneration and diabetic retinopathy. “With the proper funding to support its further utilization, the Duke Ophthalmic Registry has the potential to dramatically impact several other areas of study and clinical practices such as retina and cornea research,” says Medeiros.
The Registry has been funded through grants awarded to Medeiros—supporting his groundbreaking work in glaucoma research. Still, additional resources are needed to enable the ongoing development of the database and to allow other physicians complete access to the data.
“We hope that one day very soon the database will be available to our colleagues in other specialties, further enhancing their research and ultimately providing them with a resource that helps to address important clinical questions related to complex ophthalmic diseases,” stated Medeiros.
1Jammal et al. Blood Pressure and Glaucomatous Progression in a Large Clinical Population. Ophthalmology. 2021; In Press. DOI:https://doi.org/10.1016/j.ophtha.2021.08.021
Advancing research, education and access to eye care across the globe
For nearly two decades, Lloyd Williams, MD, PhD, a corneal specialist, has been leading global outreach initiatives to nations including Nepal, Guatemala, Zambia and Sierra Leone. Since 2001, he has made 15 trips to Africa.
The newly established Duke Global Ophthalmology Program, led by Williams, associate professor of ophthalmology, will support infrastructure, and expand global efforts by Duke Eye Center physicians.
There are at least 2.2 billion people worldwide who have vision impairment or blindness. With access to modern eye care, vision loss could be prevented or treated in at least 1 billion of those people. The world faces considerable challenges in eye care including inequalities in the coverage and quality of prevention, treatment and rehabilitation services, a shortage of trained eye care providers, and poor integration of eye care services into health systems, among others, according to the World Health Organization (WHO).
With international recognition for innovation in ophthalmology, physicians at Duke Eye Center deliver specialized care to hundreds of thousands of patients each year in Durham and surrounding area satellite clinics. Equally significant, is the commitment to delivering essential eye care and ophthalmology training to under-resourced regions around the globe.
To address eye care in underserved regions across the globe, Duke Eye Center clinicians and scientists have traveled to countries to help those in need primarily on an ad hoc basis, leveraging their own international connections.
“The newly established Duke Global Opthalmology Program will enable broader global efforts. Most importantly this work will help reduce avoidable blindness and human suffering,” said Williams.
Two dynamic missions in 2021 bear witness to the reach of Duke Eye Center and the passion of exceptional doctors.
Sierra Leone, West Africa
In July 2021, Williams returned to Sierra Leone to perform the first ever corneal transplant surgeries in the country. During this trip—delayed nearly a year due to the pandemic—he spent two days working with a local team of surgeons under his supervision, conducted eight life-changing corneal transplants which restored the vision of patients who were blind in both eyes.
Williams worked with Jalika Mustapha, MD, who leads The National Eye Programme in Sierra Leone; and John Mattia, MD and Lloyd Harrison- Williams, MD both ophthalmologists serving in the country.
Mustapha’s position allows her to invite leaders in ophthalmology, such as Williams, to come train in-country physicians in hopes that other doctors in Sierra Leone will develop the skills to conduct these surgeries, and ultimately be equipped to open and operate their own eye care facilities.
Williams relied on the local doctors to select transplant candidates who had the greatest potential for a positive outcome. The patients selected suffered blindness from result of Keratoconus or Fuchs’ dystrophy, or another factor such as a corneal scar or trauma. An additional, critical consideration in choosing the candidates for corneal transplant surgery was their ability to engage long-term in essential follow-up treatments.
One patient in particular, a mother of four, who had been bilaterally blind for nearly 30 years— and had never seen her husband or children— gained sight in one eye. It was an emotional scene for everyone when during her day-two post-op examination the woman saw her 15-year-old daughter for the very first time.

Mustapha performing life-changing corneal transplant surgery under the direction of Williams in July 2021.
“We’ve had amazing cases in the past, but never a situation as incredible as this,” Mustapha shared. “All week our patient was discovering new things, and ‘meeting’ people whom she had never actually seen before, including her husband and all four of her children. Her life was truly changed.”
Having completed hands-on surgical training with three local doctors, including Mustapha, and with nearly 20 surgeries complete, Williams carried out immediate post-op care while guiding his colleagues through specific treatment plans for each patient.
News of the successful corneal transplants traveled quickly, creating an opportunity for Williams and Mustapha to attend a meeting with Sierra Leone’s Minister of Health.
“Typically, we don’t get a lot of support for eye care in Sierra Leone,” said Mustapha. “But these surgeries really put us on the map in terms of eye health. We are so grateful for Dr. Williams’ help.”
Williams left Sierra Leone more determined than ever before to take steps that will produce progress and create hope for thousands of people in Western Africa in need of expert eye care. His aim is to grow the Duke Global Ophthalmology Program—starting with the addition of a Duke Global Ophthalmology Fellow that will go to Sierra Leone and other countries to teach and train. In addition, there is tremendous need for funding to support the purchase of ophthalmic imaging cameras that can be used in remote areas and coupled with development of a system by which Artificial Intelligence (AI) is then utilized to help diagnose and treat conditions like glaucoma, retinal diseases, etc.
“My vision for Duke Global Ophthalmology is that we’ll partner with hospitals worldwide to train and equip ophthalmologists to become skilled surgeons,” said Williams. “I am fortunate to work among so many renowned experts—each one a specialist in their unique field of ophthalmology —who are committed to improving global healthcare, and specifically eye care. I am convinced that, together, we have the potential to help eliminate blindness around the world.”
US Virgin Islands
Since residency, Grace Prakalapakorn, MD, MPH, associate professor of ophthalmology and pediatrics, affiliate faculty at the Duke Global Health Institute, and Director of International Outreach for Duke Eye Center specializing in pediatric ophthalmology, has been active in providing essential healthcare to those who need it most in a variety of places around the world, including countries in Africa and Asia.
In March of 2018, Prakalapakorn was an integral member of a health brigade hosted by the U.S. Virgin Islands (USVI) Department of Health (DOH) in collaboration with the U.S. Center for Disease Control (CDC). The brigade was deployed to the USVI to deliver recommended Zika virus-related pediatric vision, hearing, neurological and developmental health screenings to infants in the territory born to mothers with laboratory evidence of exposure to the virus during pregnancy.
Prakalapakorn led the health brigade team again in July 2021—postponed a year due to the COVID-19 pandemic—to provide ophthalmological screenings to those who were initially invited in 2018, along with others who were referred by healthcare and educational providers or in whom there were developmental concerns.
She coordinated a roster of six eyecare providers, including Duke Eye Center Orthoptist, Sandra Holgado, former pediatric ophthalmology fellows from across the country; Derek Bitner, MD, Daniel Lattin, MD and Ann Shue, MD, and Angeline Nguyen, MD from Children’s Hospital of Los Angeles, who along with other physicians, audiologists, nurses and administrative support staff delivered pediatric eye care services throughout the two-week mission. Together they granted dedicated services to more than 170 children.
“It was an honor to once again serve with the health brigade and be part of a team that was helping to meet the health and eye care needs of the children of the US Virgin Islands,” said Prakalapakorn. “I see a tremendous opportunity to bring people together from every level and function of Duke Eye Center to grow the Duke Global Ophthalmology Program in order to make a positive impact on people’s lives through education and clinical care.”
These are just two examples of global outreach that Duke Eye Center faculty led or participated in the past year.

Support for this program is essential for success. Visit DukeEyeCenter.Duke.edu/donate-and-give.
Other Duke Eye Center Global Outreach
For more than 20 years, Leon Herndon, MD, professor of ophthalmology and glaucoma division chief, has traveled to Ghana, West Africa to treat glaucoma, and has been engaged in ongoing research projects evaluating the high prevalence of primary open angle glaucoma in the region and the differential burden of glaucoma on African-derived populations. Expanding his reach in Africa, Herndon recently began collaborating with Mustapha to develop a plan for glaucoma treatment in Sierra Leone.
Victor Perez, MD, Stephen and Frances Foster Professor of Ocular Immunology and Inflammation and director of the Foster Center for Ocular Immunology, leads an international education program with events held several times a year, that offer the opportunity for ophthalmologists to learn from Duke and other international experts. Currently, they are focused on South America, with plans to expand to other regions as the Duke Global Ophthalmology Program grows.
Felipe Medeiros, MD, PhD, Joseph A.C. Wadsworth Distinguished Professor of Ophthalmology and vice chair for technology is an internationally recognized expert in the development of innovative methods to diagnose and detect glaucoma progression as well as the assessment and prevention of functional impairment in the disease. Medeiros and his team have established a one-of-a-kind database created at Duke that can help researchers conduct large-scale, complex diagnostic studies using artificial intelligence (AI) and deep learning models. The model that Medeiros and his team have created could be replicated to assist in the telemedicine plan for the Global Ophthalmology Program.
While activities have taken place and faculty have served in several different capacities, there has not been a formal, dedicated focus to the program. The strategic framework of the Duke Global Ophthalmology Program will enable Duke Eye Center to build upon decades of successful outreach, education, research, and patient care efforts and make an even greater impact on global eye health and vision.
BY VICKI FRYE
Temitope (“Temi”) Adeleke already has a number of “firsts” under her belt. She is a first generation American, the first in her family to pursue a doctoral degree and most recently, the first Underrepresented Minority in Medicine (URiM) Medical Student Summer Research Intern at Duke Eye Center.
Adeleke earned a bachelor’s degree from University of Maryland and is currently a first-year medical student at Southern Illinois University Medical School. She discovered her interest in ophthalmology shortly before finishing her undergraduate degree, while working as an ophthalmic technician at a small ophthalmology practice in Chevy Chase, Maryland. She credits the doctors and staff she worked alongside at Children’s National Hospital in Washington D.C. with encouraging her to actively pursue the practice of ophthalmology by creating opportunities for her to observe clinics and assist with hands-on patient care.
“This internship gave me an unmatched opportunity to learn from doctors who are the best at what they do—it truly solidified my passion for ophthalmology and inspired me to tap into my inquisitive nature and seek out research opportunities in this field.”
Temi Adeleke Duke Eye Center, 2021 Summer Research Intern
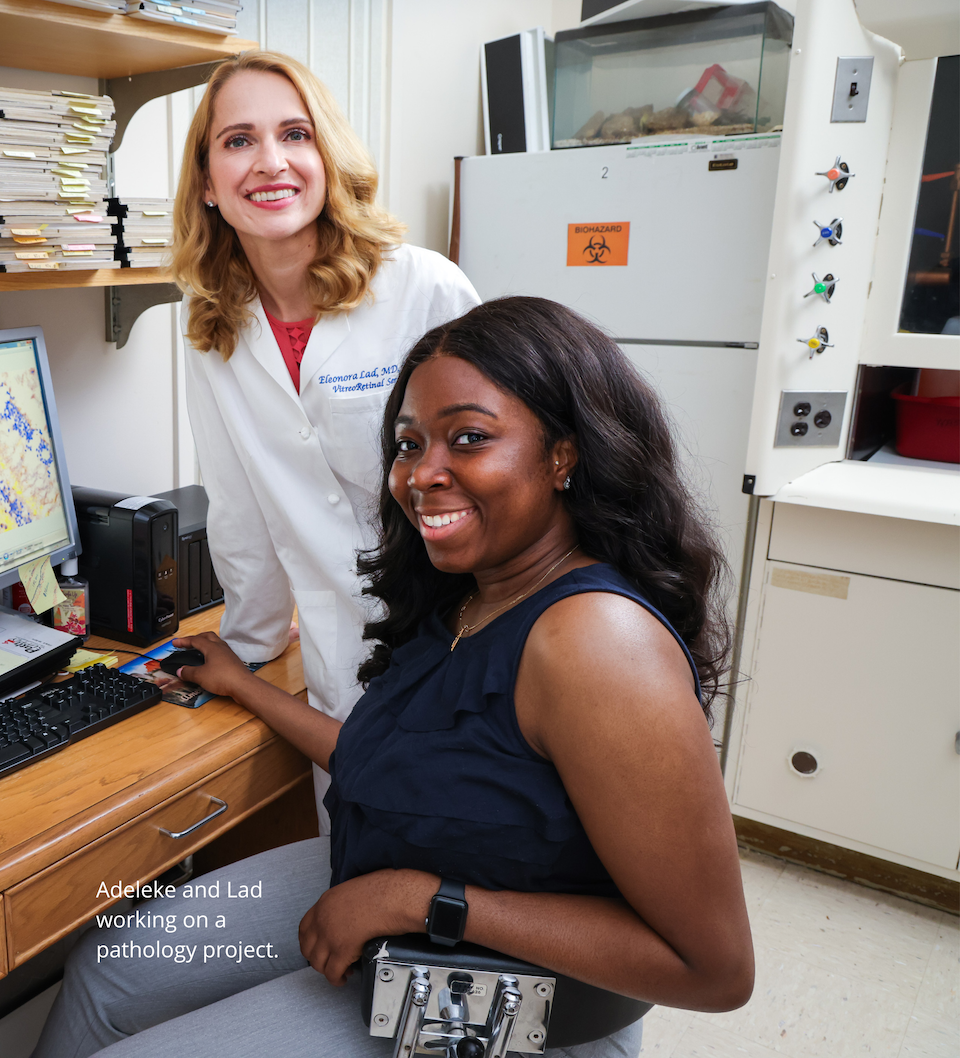
In early 2021, after applying to medical school, Adeleke joined an online community of minority students who were pursuing careers in medicine and came across an opening for the URiM Summer Research Internship at Duke Eye Center. Recognizing the importance of gaining research experience and with just days remaining before the deadline, she submitted her application for consideration. Then finally, after weeks of waiting, Adeleke received the good news that she’d been chosen to participate in the eight-week internship.
“Ophthalmology has a severe deficit of underrepresented minorities. We are thrilled to add the summer research internship to our efforts to recruit underrepresented medical students to the field,”
Goldis Malek, PhD, vice chair for diversity and inclusion in Ophthalmology.
Custom-Designed Program

The first of its kind at Duke Eye Center, the organizers of the internship program along with her mentors, structured a learning environment specifically for Adeleke—personalizing it to meet her unique goals and providing her with the chance to shadow world renowned researchers and clinician-scientists from a variety of subspecialties.
“We created an experience for Temi so that she could have a range of research exposure from basic science to translational and clinical research, since she is already familiar with the clinical care setting. It was a pleasure and honor to spend time with Temi, help her learn more about the impact of research, and mentor a future ophthalmologist,” said Eleonora Lad, MD, PhD, director, ophthalmology clinical research unit.
Prior to the internship Adeleke was completely unfamiliar with the different aspects of research and wasn’t aware of just how multifaceted it is. However, by having the occasion to move between patient care, the lab and finally on to post-mortem data analysis, she gained visibility into how it all comes together and why results-oriented research requires time and investment. Adeleke witnessed first-hand how clinical care provides data that can be analyzed and later used to shape future treatment.
“Spending time in the research laboratory setting and observing clinical faculty in clinic was an incredible honor and a true learning experience,” said Adeleke. “It allowed me to better understand the precision and compassion necessary for hands-on patient care, and showed me the fundamental relationship between basic, translational and clinical research. It was everything I’d hoped for, and then some.”

An Ophthalmologist in the Making
According to Adeleke her internship with Duke Eye Center has only bolstered her aspirations of becoming an ophthalmologist. When asked if she’s chosen a specialty in which she hopes to practice in the future, Adeleke revealed that although corneal treatments have piqued her interest, she is currently leaning toward a career in oculoplastics.
Her advice to the next Duke Eye Center Summer Research Intern?
“These doctors, who are taking the time to teach you, are not only moving the science of ophthalmology forward, but they are literally changing people’s lives,” said Adeleke. “Take advantage of the experience to study new disciplines, meet as many people as possible and keep an open mind to learn about specialties you hadn’t considered before.”
Commitment to Training URiM in Ophthalmology
Duke Eye Center is proud to have hosted the first URiM Medical Student Summer Mentored Research Program that launched in the summer of 2021 to support and help grow diversity in ophthalmology. This new program aims to catalyze the future of innovation and success of URiM students in ophthalmology.
The program was made possible by the generosity of our donors. The students selected for the program receive a paid 8-week research internship, spend time in a faculty research lab, gain clinical exposure, and benefit from discussion sessions and collaborations with our faculty and trainees. For more information on the program, please visit DukeEyeCenter.Duke.edu/donate-and-give.
BY JENNIFER BRINGLE

As a 2011 graduate of the Duke Ophthalmology Residency Training Program, Nicholas Ramey, MD, not only received the necessary training to pursue his career in ophthalmology, specializing in oculofacial reconstructive surgery, but he also enjoyed an experience and camaraderie with his fellow residents that has stayed with him a decade later.
Ramey has always felt a strong connection to the program and maintained a relationship with Pratap Challa, MD, associate professor of ophthalmology and residency program director. “My residency was the highlight of my whole educational journey,” Ramey says. With this strong connection, he knew that one day he would contribute to the experience of residents who came after him.
In thinking about his own experience in the program, he recalled a need for surgical loupes, which are magnifying devices that enhance the field of sight for accuracy and precision during surgery.
“When I was a resident, the program did not have the funds to provide loupes for each trainee. There were maybe one or two pair that the residents would share, and with 16 residents, it’s not necessarily compatible for everybody being able to use them,” says Ramey.
Some residents will pay out of pocket or find other funds to cover the cost of their own loupes. Ramey thought there might be a better way, so he reached out to Duke Health Development and Alumni Affairs to discuss supporting the residency program by providing loupes to all residents.
Ramey provided a generous gift to the Duke Residency Program in 2021 that supports each resident getting their own pair of loupes. Residents should be able to use the devices long after they complete residency training.
“Dr. Ramey’s gift provides a tremendous opportunity for our residents. We are grateful that the program means so much to him.”
Pratap Challa, MD Duke Ophthalmology Residency Program Director
Now that the fund is up and running, it has grown to include other educational needs.
“It’s not just a loupes fund but a fund to support resident education,” Ramey says. “The first year, none of the residents had their own loupes, so it was a big outlay to bring 18 residents up to speed. I’m still donating the same amount for the next several years, so only the incoming six residents will need them, which means two-thirds of the money will go to other things like microscopes.”
Ramey says his only regret about giving is that he didn’t do it sooner. He felt he had to reach a certain point in his career to give a larger amount, but he now realizes that even smaller gifts can have a big impact.
“Even if it’s not a huge gift, anything really can help,” he says. “I would advise people to touch base with the department early and start the conversation, whether you feel you’re fully ready for it or not, because it can be productive even if you’re not at the level you envision.”
Ramey says he’s grateful for the opportunity to help give future residents the same life-changing experience he had at Duke.
“I’m just happy and proud to be part of the program that gave me so much, and hopefully this will help others have that same experience,” he says.


For more information on how you can support Duke Eye Center, please visit DukeEyeCenter.Duke.edu/donate-and-give.
with New Mobile Imaging Van

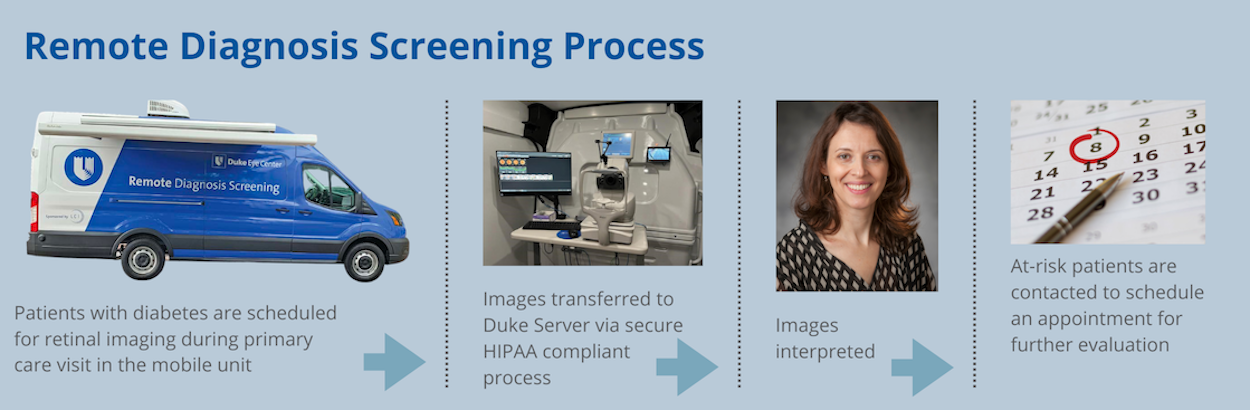
Duke Eye Center recently established a mobile eye imaging center—a van that has been modified and equipped to screen patients at primary care clinics to identify eye disease. This advancement in remote diagnostics became reality from a passionate focus of Scott Cousins, MD for access to eye care and a generous gift from LC Industries Foundation.
Access to healthcare is a major unmet need and heightened because of the COVID-19 pandemic. Poor access, especially for people with diabetes, can lead to blinding eye disease due to delayed diagnosis and care for diabetic retinopathy (DR), which is present in more than two million diabetics in the U.S. It is estimated that only 40-50% of patients adhere to American Diabetes Association guidelines for screening, and only half of those are between patients and given an appointment or appear in clinic for a dilated eye exam. Early detection of diabetic retinopathy allows early intervention to slow or even stop vision loss caused by DR.
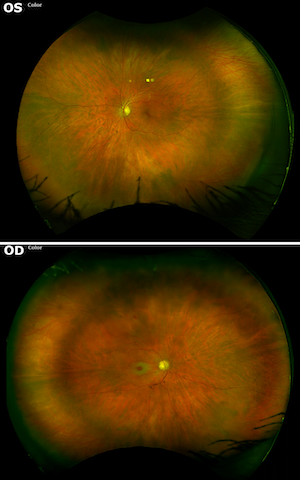
Cousins, Robert Machemer, M.D. Professor of Ophthalmology, developed the concept for remote diagnosis that uses a combination of color fundus photo (CFP) and optical coherence tomography (OCT), two complementary types of eye imaging, on non-dilated pupils to image the retina. The remote screening approach can be performed by non-expert imagers, using less expensive equipment, at a location that is convenient to the patient and the primary care doctor. This provides an accessible, efficient, low-cost screening option, which improves outcomes and patient satisfaction.
“Improvements in eye imaging technology now make remote diagnosis a feasible real-world alternative to an annual dilated eye exam. Our research shows this approach to be as effective as a traditional examination for identifying DR. The LC Industries Foundation gift has made possible the potential to change the way eye diseases are diagnosed and managed in the future,” said Cousins.
The new mobile unit equipped with necessary imaging equipment is parked outside of a primary care office, and images are taken in the van and electronically transferred to a cloud-based storage system that can be accessed by graders at a HIPAA-compliant reading center. Images are read by ophthalmologists, and at-risk patients are contacted by a member of the Duke Eye Center staff to schedule an appointment with retinal specialist for further examination. An automated image interpretation tool with a deep learning model is in development, and early research shows it to be as effective as a human image reader in identifying diabetic retinopathy.
Majda Hadziahmetovic, MD, assistant professor of ophthalmology, is leading the academic effort of the program in conjunction with Cousins and Prithu Mettu, MD, assistant professor of ophthalmology who oversee the operations.
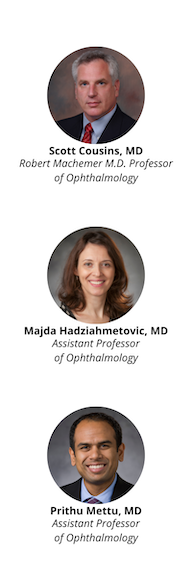
“Our studies have demonstrated feasibility of this innovative diagnostic approach, with the goal that remote diagnosis becomes standard of care in early diagnosis and monitoring of many sight-threatening diseases,” said Hadziahmetovic.
LC Industries Foundation is led by William Hudson and has provided significant funding over the years to Duke Eye Center for research and patient care for the prevention of eye disease. The Foundation is the primary benefactor of the state-of-the-art clinical pavilion that is named the Hudson Building at Duke Eye Center, which opened in 2015. The gift from LC Industries Foundation to support this project has provided not only the vehicle and equipment, but also the ability to collect more data and further show the impact of remote diagnostics in eye care.
“Having a way to assess people for blinding eye disease at their convenience by bringing the screening to them, I think this is a real game-changer,” said Hudson. “Hopefully, this approach can lead to early intervention to slow or stop vision loss among people at risk for eye disease.”
BY TORI HALL
Reducing the Impact of Vision Loss
The Duke Eye Stroke Clinic opened in August 2021 for patients who have experienced eye stroke and are beyond the emergency phase of their care. It offers expertise in neurology and neuro-ophthalmology paired with advanced vision testing capabilities in one location. The clinic, combined with Duke’s leading emergency hyperbaric medicine services and vision rehabilitation center, offers a comprehensive approach to eye stroke care.
Co-led by Chantal Boisvert, OD, MD, associate professor of ophthalmology and neuro-ophthalmology division chief and Brian Mac Grory, MB, BCh, MRCP (UK), assistant professor neurology and the 2020 recipient of the American Heart Association/American Stroke Association Stroke Progress and Innovation Award for his research examining treatment for CRAO.
This distinctive multidisciplinary clinic specializes in the treatment of patients with central retinal artery occlusion (CRAO) and other strokes affecting vision pathways in the brain and has the potential to dramatically reduce the burden on people affected by eye stroke. The collaboration helps to clear communication among the specialists on a patient’s care team.
The Duke Vision Rehabilitation and Performance center, led by led by Division Chief, Diane Whitaker, OD, assistant professor of ophthalmology and includes dedicated ophthalmic occupational therapists to help patients address performance challenges in activities of daily living and functional mobility following the loss of vision in one eye. Patients are referred to Whitaker or an occupational therapist following their treatment in the Eye Stroke Clinic.
“We are excited to offer this unique combined clinic that will improve the care of patients suffering from retinal artery occlusion—two specialties seeing patients on the same day in the same clinic not weeks apart, provides a convenience for the patient and allow us to manage the patient more effectively—together.” says Boisvert. Having vision rehab in the same building is an added benefit for our patients to help them learn to live a normal life with vision in one eye.”
Emergency Treatment—Key to Impact on Vision Loss
Most strokes present with weakness, facial droop, or difficulty speaking. Eye strokes are hard to recognize and treat in a timely manner because the only symptom may be sudden blindness in one eye. Patients with sudden vision loss should immediately go to the ED before seeing a PCP or specialist to reduce the impact of the sudden vision loss.
“When we think of strokes, we think of obvious symptoms, but eye strokes are a hidden menace; they do not have any of the symptoms that most people associate with stroke,” Mac Grory says.
Duke is fortunate to have a large multidisciplinary emergency team capable of delivering advanced therapies—including a premier hyperbaric oxygenation program. Perhaps most importantly, the Duke telestroke network and ambulance/helicopter capabilities mean we can rapidly transfer patients from other parts of North Carolina and surrounding states to receive these treatments.

Eye Stroke Detection—Vascular Conditions and Risk of Future Stroke
Boisvert and Mac Grory collaborated together on a study published in the August 2021 issue of Stroke, that demonstrated eye stroke may be the first sign of atrial fibrillation, a common, underdiagnosed heart rhythm problem that is associated with an increased risk of future stroke.
“The rate of AF detection after CRAO is higher than that seen in people without CRAO but who are otherwise the same in terms of age and risk factor profile and comparable to that seen after a person has an ischemic cerebral stroke,” Boisvert and Mac Grory explain. “Paroxysmal AF should be considered as part of the differential etiology of CRAO, and those patients may benefit from long-term cardiac monitoring.”
Research and training for residents and fellows are also among the priorities. Mac Grory and Boisvert are establishing a detailed registry of patients with eye stroke which will provide sorely needed data on the long-term impact of eye strokes, the effect of treatment and the risk of future stroke.
Boisvert and MacGrory hope that the Duke Eye Stroke Clinic can lessen the impact and improve overall health for patients suffering from eye stroke in the North Carolina region, and create a model for other multidisciplinary centers to establish a similar approach to make progress in outcomes of eye stroke care across the country.
With the Help of a Nurse Turned Pioneer in Clinical Design

Duke Eye Center opened a 14,000 square foot clinic in May 2021 located in the new Duke Health Arringdon, a multi-specialty clinical facility that includes an ambulatory surgery center (ASC) for a wide range of outpatient surgery.
The new state-of-the art Duke Eye Center clinic offers cornea, glaucoma, and retina subspecialties, features 25 eye lanes, six rooms for injections and lasers, minor surgical procedures, as well as a large room for laser refractive surgery.
The open-concept design includes workspace areas to encourage relationship and team building, as well as plenty of natural light and beautiful landscape views of Morrisville and Research Triangle Park. The Duke Ambulatory Surgery Center located on the fifth floor of the building will serve patients that require surgical procedures.
Duke Eye Center Arringdon, like other satellite locations, aims to bring multiple specialties to patients in their own communities to meet the needs of the exponential growth of the region. This is the sixth satellite clinic for Duke Eye Center. Additional clinics are planned to span across the region in the coming months and years.
Arringdon was designed with the help of Kim Denty, RN, MSN, a pioneer in clinical design and an expert in patient safety. She has assisted with the design of six clinics for Duke Eye Center, from upfitting new to remodeling existing space. With each project, she adheres to a common theme—commitment to a safe, functional, environmentally friendly, cost-effective clinic to enhance the patient experience and make delivery of care more efficient.
“We have been so fortunate to have Kim’s expertise when designing our clinics. She is amazing and really does take the whole operation into consideration. Each clinic has Kim’s unparalleled touch and attention to detail. We could not be prouder of what she has done to make our clinics as efficient, safe, and economical as possible,” says Heidi Campbell, COT, director of operations for Duke Eye Center.
Denty began her career as a staff nurse and then held administrator roles in the Cancer Center at Duke Health. She has a passion for clinical design—even if she didn’t quite know it when she started as a staff nurse. At the time, the Cancer Center was in Duke South, the original home of Duke University Hospital. Denty remembers struggling with her daily work due to the clinic’s inefficient design. What she realized is that most building architects do not have clinical operations experience and do not fully understand why it is so important to pay attention to certain details.
“When I worked in clinic, I was always taking things apart, moving walls, moving equipment to help patients and staff maneuver in the clinic,” she describes. The rooms were small and made it difficult to perform patient care—it became extremely challenging in a space that could barely accommodate patients, their families, physicians, residents, and nurses.

Denty continued to enhance facilities while also working in clinical administrator roles and as a patient safety advocate.
When the opportunity came along for her to become the Associate Vice President for Clinical Site Development and Patient Safety for the Private Diagnostic Clinic (PDC), the physician practice of Duke Health, Denty jumped at the chance to spend her days making clinics safer and more comfortable for both patients and providers. While in the site development role, Denty has been responsible for designing multiple new Duke Health multi-specialty buildings which totals hundreds of thousands of square feet. Arringdon alone has 70,000 square feet of clinical space.
Denty retired in November 2021 to slow the pace of hectic long hours and reflect on the positive impact she made at Duke.
“We will miss Kim being a part of our clinical designs going forward but are forever grateful for the extraordinary expertise she has shared to improve the patient experience,” says Eric Postel, MD, professor of ophthalmology and vice chair for clinical affairs.
Denty approaches clinical designs as an all-inclusive effort—considering efficiency of operations, providers, staff, but ultimately, decisions are made based on patient care, safety and patient feedback, and long-term goals of the clinic.
“For me, it’s always been about patients, and when I think about a clinic—how patients get around clinics, whether they’re in a wheelchair, on crutches, visually impaired, or just walking normally,” Denty said. “Everything begins with the patient, and it always begins with the front door, all the way through to the end when they check out.”
For instance, Denty will “light the way” down long hallways and in exam rooms and using contrasting flooring to help low-vision patients navigate the clinic.
Another aspect of clinic design involves ensuring a good return on investment. Some examples include, installing sliding “barn doors” for exam lanes which reduced the amount of space needed for a traditional door to swing open, which in turn allowed for an increased number of exam lanes in the clinic. She selects sustainable materials for flooring and furniture to easily clean and sanitize and reduce ongoing maintenance and chemical footprint. She implemented an electronic fire extinguisher monitoring system to maintain fire extinguisher records that used to be handled by staff, which took them away from patient care.
- Contrasting flooring, handrails, and other ADA compliant safety features for fall prevention
- Exam chairs that glide and can be moved to accommodate a wheelchair
- Sliding barn style doors to maximize space in the exam lanes
- Comfortable soothing color scheme to put patients at ease
- Use of sustainable materials to reduce chemical footprint and long-term cost savings
Although each new clinic presents a new challenge, Denty says she feels fortunate to have the opportunity to impact so many clinics at Duke. She also encourages others with a clinical background to think about how they can apply their skills to facility design.
“I know it doesn’t sound exciting for nursing to get involved in architecture or construction, but I’ll tell you, I don’t think there’s a more important job,” she says. “I love the fact that when I walk into a clinic, and I see patients comfortably sitting in chairs, that I feel like I was a part of helping them to get safe, quality health care in a great environment,” says Denty.

A Bright Future in Sight

The Duke Ophthalmic Technician program is an excellent opportunity for individuals who are interested in a direct patient care role. Following completion of this accelerated one-year, full time program, graduates are prepared to take the Ophthalmic Technician certification exam, guaranteed financial security and have a variety of career options.
The field is currently experiencing a severe national shortage, creating a high demand for ophthalmic technicians in ophthalmology practices. More than 90% of Duke Ophthalmic Technician program graduates secure a position within a month of graduation and have excelled in their careers; becoming team leads, clinical operations managers and ophthalmic photographers, among other eye care and leadership roles.
Benefits of the program:
- Students may begin the program after earning a high school diploma; students must be 18 at start of clinical rotations
- No college degree or prerequisites required
- Earn a certificate in one year with eligibility to take the ophthalmic technician certification exam
- Nine months of hands-on experience in clinical rotations at Duke Eye Center clinics
- Starting pay after program completion and earning a certification can be $22-$24/hr
- Tuition is affordable compared to other allied health programs and financial aid is available
Individuals of all ages and stages of their career interested in an allied health career that does not require a four-year degree are encouraged to apply.
Visit dukeeyecenter.duke.edu/optech for more information and application instructions. Email optech@duke.edu with questions.
From a Recent Graduate

“The Duke OpTech program is fast paced with amazing opportunities to learn from the very best. The year was filled with growth in every way as I learned under the direction of the most capable and talented mentors. I loved the varied experiences that created challenges to grow every day. I would recommend the program to anyone that desires to jumpstart into a healthcare career that will be rich with challenges and rewards. I am so excited to start this career and I feel confident as I know I had the very best education and training to prepare me for this.”
- Olivia Guy, Class of ‘21
She believed she could, so she did.
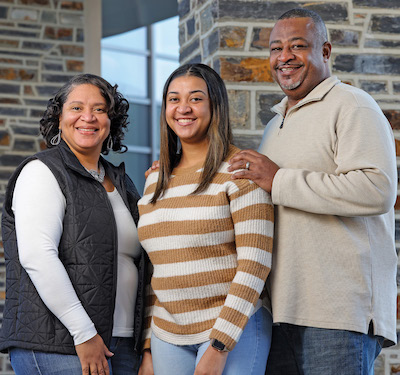
That’s the motto of Wilicia McClendon, now 21, who is fierce with determination despite living with Usher Syndrome. She has her sights set on completing her undergraduate degree and opening a daycare to serve children living with disabilities.
Wilicia’s parents, Wilbur and Alicia McClendon, learned their daughter was profoundly deaf at a year old. At age 10, she began having trouble with her vision. Doctors predicted their daughter would be blind by early adulthood, and nothing could be done to save her vision.
The McClendon’s are no stranger to challenges, their home was destroyed by Hurricane Katrina in New Orleans, and they relocated to Laurel, Mississippi. No matter the obstacles they faced, Wilbur and Alicia were not going to accept this diagnosis, and they set out on a mission to save her sight.
Wilicia was ultimately diagnosed with Usher Syndrome, a rare, inherited genetic condition that affects hearing and vision. A major symptom is retinitis pigmentosa (RP) a form of inherited retinal degeneration (IRD) that causes night-blindness and peripheral vision loss through the progressive degeneration of cells in the retina.
They began to research doctors that treat Wilicia’s condition and found Alessandro Iannaccone, MD, FARVO—an international expert and one of few ophthalmologists in the world who treats RP and IRDs—while he was practicing in Memphis, Tennessee. At Wilicia’s first appointment, they were relieved to learn that Iannaccone felt he could help slow severe vision loss. She began a regimen of retinal injections, dietary supplements and vitamins that have shown to mitigate, at least in part, the rate of disease progression.
“If we had accepted what her other doctors said and moved on, I can only imagine where Wilicia would be today,” said her father, Wilbur. “Alicia and I wanted to make sure our daughter had the best available care, so that’s what we set out to do.”
Iannaccone, joined Duke Eye Center in 2017 to launch the Duke Center for Retinal Degenerations and Ophthalmic Genetic Diseases. The McClendon’s were so impressed with the care he provided in Memphis, they will follow him wherever he goes, no matter how far they must travel.
“Wilicia’s condition, Usher Syndrome type 1, is a progressive disease that has significantly affected her vision. We have been fighting to keep it under control by taking advantage of the results of clinical trials and other research that have identified treatments to slow rate of progression,” said Iannaccone.

After gaining control of disease progression, the next step was to discover the cause for her condition. At Duke Eye Center, broader genetic testing is available and was used to help discover the cause for her condition. This allows Wilicia to become eligible for other treatment options and for gene therapy which is expected to become available in the near future.
“By discovering the exact type of genetic changes at play, we now also know that a special category of investigational medications, known as translational readthrough-inducing drugs, or TRIDs, could be potentially used to treat Wilicia’s condition," said Iannaccone.
The third step in her treatment was to bring the inflammatory component to her condition under better control. This too proved challenging initially and caused some important and rapid vision loss in one eye, but over the past several years it has been under far better control her condition has stabilized.
The opportunity for Wilicia to enter a clinical trial may be a true game changer. While clinical trials are a good-faith, evidence-based attempt to find a cure or a new treatment for a problem, there is a chance they may be unsuccessful. When faced with the prospect of incurable progressive vision loss, trials represent an incredible beacon of hope for IRD patients. “We have the moral obligation to try as hard as possible to bring available trials to these patients. I have been working on IRDs to get to this point for more than 30 years, and I remain committed to this goal now more than ever,” said Iannaccone.

Today, Wilicia is a student at the University of Southern Mississippi (USM), where she is pursuing a Bachelor of Science degree in child and family science. She transferred to USM after graduating from Jones College in May 2021 with two associates degrees.
College has presented a new set of challenges for Wilicia, but it has not deterred her. “I just have to keep pushing, and one day I will have my own daycare for children with disabilities—inspired by her mother’s struggle to find a daycare when she was growing up,” she said.
“Being an advocate for Wilicia has taught us to speak to other parents of kids with not just hearing and vision problems but speech and other disabilities. We tell all of them, speak for your child.”
Alicia McClendon
The McClendon’s perseverance, along with the help of Iannaccone and other specialists, have helped Wilicia overcome predictions that she would be severely disabled and unable to lead a normal life.
Wilicia can now advocate for herself, but her parents continue to be a driving force in her success by supporting her goals with her best interests in mind, standing in the background in case she needs them. “Being an advocate for Wilicia has taught us to speak to other parents of kids with not just hearing and vision problems but speech and other disabilities. We tell all of them, speak for your child,” Alicia said.
Most importantly, Wilicia is committed to speaking up, “I can’t let my disability stop me,” she said.
Portions of this article have been reprinted with permission from The University of Southern Mississippi.
Sonja Beach visited Duke Eye Center for a consultation as a last resort in September 2020 after having almost unbearable pain and light sensitivity in her right eye and being treated for an eye infection by her primary care provider. She was familiar with the symptoms, because in 2010 she had an intracorneal ring segment (ICRS) removed from her left eye due to the similar discomfort. This time it was different though, there was a lot more pain, and she was experiencing severe light sensitivity.
Beach initially elected to have bilateral ICRS implants in 2000 to help her nearsightedness, just as the technology was beginning to emerge.
Upon her initial visit at Duke Eye Center, she was told that the implant would need to be removed—holes had developed in her cornea, which were the cause of the pain and light sensitivity she was feeling.

“My first thought was, I’m going to go blind,” Beach remembers thinking after hearing the news. She was assured that she would not go blind but may have some permanent damage to her eye, and was referred to Duke corneal surgeon Lloyd Williams, MD, PhD for a consultation.
The next day, Beach was surprised to hear from Williams’ scheduler Tina Mazzurco, COT who happened to review her chart that morning and noticed that her case was severe, and that she needed to come as soon as possible for the ICRS removal.
Beach returned to Duke for surgery two days later and felt instant relief after the procedure. “I just cried because I was just so relieved,” she said.
Problems with ICRS do not happen frequently and removal is not typically revolutionary or surprising. “Ms. Beach is the only patient I have ever seen with a significant problem from ICRS. What stood out immediately upon seeing her is the deep hole in her cornea extending all the way down to the ICRS. It is very uncommon to see so deep a lesion without infection or severe inflammatory disease,” said Williams.

Following the procedure at Duke, it appeared that she was making good progress and her eye was healing until she felt the same pain and irritation again.
Williams discovered that Beach’s eye had epithelial ingrowth into the channel where the ICRS had been located after removing it. The ingrowth was causing pain, decreased vision, and inflammation with some new corneal melting. He had never seen a case like this before, so he did some research before approaching treatment. “We spent some time looking for papers or reports on how other ophthalmologists did this and didn’t find anything, so we had to figure it out using surgical and engineering principles,” said Williams.
Williams decided to treat the epithelial ingrowth into the channel by performing a washout of the channel with saline. He made a cut down at both ends and flushed the channel from one end to the other and then sutured the floor of the channel to the roof of the channel while at the same time closing the incisions. After several schematics, Williams and his team came up with a good drawing of how the mechanics of the situation worked and how exactly to perform the procedure without creating any new problems or decreasing her vision.
That part of the journey was the part that was so unique because a case like this had not been documented anywhere.
“That’s where his pioneering mindset and his ability to think through and solve a problem that had never been solved came into play.”
Sonja Beach
It was only later that Beach learned she had been potentially days away from losing her sight.
Williams has experienced nearly losing his vision.
“I found that I felt like I was losing more than just sight, I was losing who I was. Although all people are different, I have always assumed that patients have a similar anxiety about losing vision. Overall, I think my own experiences have added empathy to how I view patients.”
Lloyd Williams, MD, PhD
Thanks to Williams’ pioneering intervention, Beach’s irritation is gone, and her vision is better than ever. “I can see better now than I’ve ever seen,” she says. “I don’t even need reading glasses anymore.”

Corina Busuioc, OD joined us from Northwell Health Department of Ophthalmology in Great Neck, NY where she specialized in specialty contact lenses and the PROSE treatment. She graduated from the University of Houston College of Optometry (UHCO). She also completed a Cornea and Contact Lens Fellowship at UHCO and a PROSE Fellowship at BostonSight. Busuioc sees patients for the PROSE treatment, scleral lens fits and Dry Eye treatments in the Foster Center for Ocular Immunology.
Tanya Glaser, MD joined Duke Eye Center faculty after completing fellowship in Pediatric Ophthalmology and Strabismus at Duke Eye Center. She also completed ophthalmology residency and served as Chief Resident at Duke. Glaser earned her medical degree at University of California, San Francisco. Her clinical and research interests are in childhood glaucoma, cataracts, and the management of children and adults with ocular alignment issues, called strabismus, and treatment of amblyopia. When a patient and their family visits her clinic, she wants them to leave having had as much fun as possible and feeling empowered and knowledgeable about their eye issue. Respect is an important part of her patient interactions, and she uses each visit as a chance to further develop a long-term relationship. When not at work, Glaser spends time with her family. They enjoy outdoor activities, such as swimming, hiking, and gardening. She also enjoys painting, pottery, and doing art projects with her child.
Amber Hoang, MD is a fellowship-trained, board-certified ophthalmologist with expertise in the treatment of corneal and anterior segment diseases. She performs routine and complex cataract surgery including laser assisted cataract surgery and implantation of astigmatism and presbyopia correcting intraocular lens. Hoang specializes in the treatment of corneal diseases including crosslinking, PKP, DSAEK, and DMEK. She performs anterior segment surgeries including pterygium excision, iris reconstruction, and secondary intraocular lens implantation. She offers laser eye surgery including custom bladeless Intralase LASIK, PRK, and PTK. She has a special interest in the management of ocular surface diseases like dry eye and blepharitis. She offers new treatments including Lipiflow, TearCare, Blephex and intense pulsed light therapy (IPL). Hoang has authored many articles in peer-reviewed literature and has also written multiple textbook chapters about corneal disease. She is an active member of the American Society of Cataract and Refractive Surgery (ASCRS), Women in Ophthalmology (WIO), and American Academy of Ophthalmology (AAO).
Kourtney Houser, MD joined us from Hamilton Eye Institute at University of Tennessee Health Science Center in Memphis, TN. She completed her cornea fellowship in the Cullen Eye Institute at the Baylor College of Medicine in Houston, TX. Houser completed residency training in ophthalmology at Tennessee Health Science Center, where she also earned her medical degree. Her clinical interests include corneal transplantation (ie. PRK, DALK, DSEK, DMEK), corneal collagen crosslinking, complex cataracts, IOL exchange, cataract surgery with advanced technology, including presbyopia correction and laser-assisted surgery and refractive surgery (ie. LASIK, PRK, RLE).
Amol Sura, MD joined Duke Eye Center after completing sub-specialty training in uveitis and ocular immunology at the F.I. Proctor Foundation/University of California, San Francisco. Sura completed residency training at the University of Alabama, Birmingham. He joins Victor Perez, MD in the Foster Center for Ocular Immunology, where his clinical interests include all varieties of uveitis, scleritis, cicatricial pemphigoid, inflammatory ocular surface diseases, and cataract surgery. In his free time, he enjoys farmer’s markets, biking, and eating the samples at Costco.
N. Troy Tagg, MD joined Duke Eye Center from The Uniformed Services University and Walter Reed National Military Medical Center in Bethesda, MD. He completed his Neuro-Ophthalmology fellowship in the Department of Ophthalmology and Visual Sciences at The University of Iowa in Iowa City, IA. Tagg completed residency training in neurology at Walter Reed Army Medical Center (Washington, DC) and National Naval Medical Center (Bethesda, MD). He earned his Doctor of Medicine degree from the University of Iowa Carver College of Medicine. His interests include autoimmune conditions that affect vision (neuromyelitis optica, multiple sclerosis, myasthenia gravis, etc.), vascular disorders, and pseudotumor cerebri, among others.
New Vice Chair Appointments
Diversity and Inclusion
Goldis Malek, PhD, associate professor of ophthalmology, is the inaugural Vice Chair for Diversity and Inclusion at Duke Ophthalmology. Malek has an outstanding record in diversity, equity, and inclusion, having served as the department’s Chair for Diversity Equity and Inclusion Council. Malek is a principal investigator whose laboratory focuses on understanding the cellular and molecular pathogenic mechanisms underlying the dry and wet forms of AMD, with the goal of identifying potential therapies. In the role as vice chair, she will advocate for new diversity-related programs and activities that align with the goals of the department.
Research

Cynthia Toth, MD, Joseph A.C. Wadsworth Professor of Ophthalmology has been appointed Vice Chair for Clinical Research. Toth specializes in the evaluation and surgical treatment of vitreoretinal diseases in infants, children, and adults, and in novel research resulting in the clinical application of optical coherence tomography (OCT) imaging in surgery and at the bedside. She brings a wealth of experience to the position and is passionate about taking the Duke Ophthalmology clinical research programs to the next level.
Vadim Arshavsky, PhD and Dan Stamer, PhD have been appointed Co-Vice Chairs for Basic Science Research. Both are leaders in their respective scientific areas, who will help chart a future path for the basic science program at Duke Ophthalmology.
Arshavsky, Helena Rubinstein Foundation Professor of Ophthalmology, studies cellular pathologies that cause loss of vision in patients suffering from inherited retinal degenerations. His research explores therapeutic approaches that would prevent the disease or reverse its progression.
Stamer, Joseph A.C. Wadsworth Professor of Ophthalmology and past president of Association for Research in Vision and Ophthalmology (ARVO). His laboratory studies the disease of glaucoma, with the goal of finding more effective ways to medically control intraocular pressure by targeting the conventional outflow pathway.
NEW STUDY SHOWS PROMISE FOR GEOGRAPHIC ATROPHY
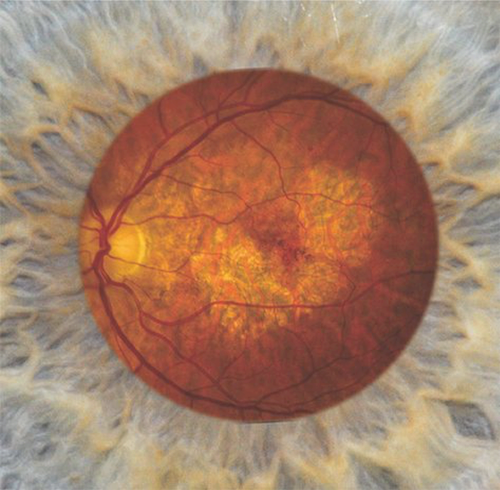
Recently announced top line results from Apellis Pharmaceuticals, Inc phase 3 OAKS trial, shows potential for intravitreal pegcetacoplan to become the first treatment for patients affected by Geographic Atrophy (GA) secondary to age-related macular degeneration, a leading cause of blindness worldwide. There are currently no approved treatments for GA.
Duke Eye Center serves as an international lead site for the Apellis phase 3 OAKS trial, led by Eleonora Lad, MD, PhD as principal investigator, vitreoretinal division faculty co-investigators (Michael Allingham, MD, PhD; Scott Cousins, MD; Sharon Fekrat, MD; Dilraj Grewal, MD; Majda Hadziahmetovic, MD; Prithu Mettu, MD; Stefanie Schuman, MD; Lejla Vajzovic, MD; and fellow Oleg Alekseev, MD, PhD) and our outstanding clinical research unit team.
“These top line results of the 3 OAKS trial are a pivotal milestone in treatment for irreversible GA. The first clinical trial to show promise and the potential to become an FDA-approved treatment for GA. It is so rewarding to lead our site and participate in this transformative trial that may help our patients and offers hope for those with blinding retinal disease,” said Lad.

GA is an advanced form of age-related macular degeneration (AMD), a leading cause of blindness. GA is progressive and irreversible, leading to central visual impairment and permanent loss of vision. Based on published studies, more than five million people have GA globally, including approximately one million people in the United States.
Pegcetacoplan is an investigational, targeted C3 therapy designed to regulate excessive activation of the complement cascade, part of the body’s immune system, which can lead to the onset and progression of many serious diseases. Pegcetacoplan was granted Fast Track designation by the U.S. Food and Drug Administration (FDA) for the treatment of geographic atrophy.
Results of the 3 OAKS trial continue to be analyzed and further results and detailed data will be presented at upcoming scientific meetings.
OSTEOPONTIN: A NEWLY IDENTIFIED BIOMARKER FOR EARLY AGE-RELATED MACULAR DEGENERATION

Age-related macular degeneration (AMD) is the leading cause of vision loss in the elderly in the Western World. The dry clinical sub-type of this disease occurs in approximately 85% of patients and is characterized by the accumulation of extracellular deposits in the posterior pole of the eye. The exact mechanisms involved in the growth and development of these deposits, which are similar to those that form in systemic and neurodegenerative diseases such as atherosclerosis and Alzheimer’s disease, is not known. Additionally, there are no therapies available to patients with dry AMD.

In a recent study, published in journal of Modern Pathology, Goldis Malek, MD, PhD and team identified a new histological biomarker of deposits in the posterior pole called osteopontin, a multi-functional protein involved in the recruitment and retention of immune cells. Additionally, they report that when ocular cells are exposed to oxidative stress, they are capable of secreting this protein, thus identifying a mechanism potentially contributing to the formation of deposits in the back of the eye. Future studies will explore whether or not osteopontin could be effectively targeted as a potential therapy for age-related macular degeneration.
RACIAL DISPARITIES IN RETINAL VEIN OCCLUSION

Retinal vein occlusion is the second most common cause of acquired retinal disease. Two companion papers—one authored by medical student, Justin P. Ma, BS, at Duke University and the other by ophthalmologist Sieh Yean Kiew, MBChB, M Med(Ophth), FRCOphth, FAMS at Duke- National University of Singapore—are part of collaborative work spearheaded by Duke retina specialist Sharon Fekrat, MD, FACS, FASRS.
The findings, which appeared in Ophthalmic Surgery Lasers Imaging Retina [branch retinal vein occlusion (BRVO); Ma, 2021] and the Journal of VitreoRetinal Diseases [central retinal vein occlusion (CRVO); Kiew, 2019], assess the effect of race on the presentation, treatment, and outcomes in eyes with retinal vein occlusion.
Both studies evaluated a large, racially diverse cohort from Duke Eye Center, placing them amongst the most diverse studies to examine this subject. Data on demographics, comorbidities, treatment rates and types, time to treatment, visual acuity, and clinical imaging signs were collected.
Of those 285 persons with BRVO, African American patients were more likely to have diabetes and open angle glaucoma; however, there were no differences in management or outcomes between patients of African American race and those of other races. Of those 479 individuals with CRVO, African American patients were older and presented with worse visual acuity and were more likely to have hypertension, diabetes, and open angle glaucoma.
In African American patients with treatment-naïve CRVO, there was a higher treatment burden, evidenced by more anti-vascular endothelial growth factor injections, during the first 12 months. Further study will allow us to learn more.
LINK BETWEEN THE RETINA AND THE BRAIN IN PARKINSON’S DISEASE

The Eye-Multimodal Retinal and Choroidal Imaging in Neurodegenerative Disease (iMIND) group at Duke Eye Center has published two studies identifying a link between the retina and the brain in Parkinson’s disease. The iMIND group uses multimodal retinal and choroidal imaging including optical coherence tomography (OCT) and OCT angiography (OCTA) to identify changes in small vessels that may be associated with neurodegeneration.
Parkinson’s disease is associated with neurodegeneration in multiple regions of the brain. Cason Robbins, MD, PGY1 at Duke Eye Center, was lead author on the studies and was mentored by Sharon Fekrat, MD, professor of ophthalmology and Dilraj Grewal, MD associate professor of ophthalmology who lead the iMIND group.

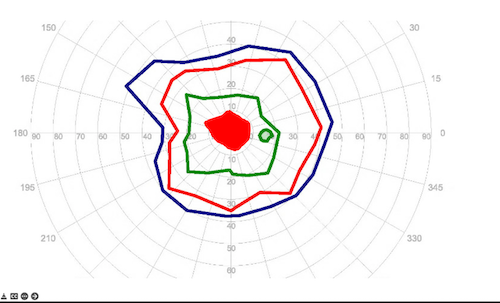
Robbins and collaborators found that individuals with Parkinson’s disease had decreased retinal vessel density and perfusion density on OCTA as well as increased total choroidal area, choroid luminal area, and decreased choroidal vascularity index (a ratio of choroid luminal area to total choroidal area) compared to healthy controls. These findings, published in JAMA Ophthalmology, suggest that individuals with Parkinson’s disease might have changes in the retina that mirror changes seen in the brain.
In a second study the iMIND group analyzed differences in the peripapillary microvasculature (i.e. capillaries surrounding the optic nerve head) in individuals with Parkinson’s and healthy controls. This study Robbins and collaborators published in Ophthalmology Retina, showed that individuals with Parkinson’s disease had increased peripapillary capillary perfusion density compared to healthy controls. This difference held true after adjusting for age and sex as covariates, and was not associated with a change in retinal nerve fiber layer (RNFL) thickness, suggesting that microvascular changes in Parkinson’s disease may occur prior to thinning of the RNFL which has been suggested in some prior studies utilizing OCT.
In these two studies, the authors hypothesize that neurodegeneration related to abnormal protein accumulation in Parkinson’s disease may impact the retina, as prior studies have shown alpha synuclein (the pathologic protein of Parkinson’s) accumulating in the retina. The death of nerve cells in the retina may be associated with a change in the retinal vasculature which is visualized using OCTA. OCTA is beneficial for screening for neurodegenerative disease as it is non-invasive, easy to acquire, and may be useful for long-term monitoring/progression.
Future studies are underway to analyze the longitudinal changes on OCTA in Parkinson’s disease, which may yield further insight into OCTA as a biomarker for both diagnosis and disease progression. These studies have shown that, in neurodegenerative disease, the eye is truly a window to the brain.
UPDATES IN PEDIATRIC OPHTHALMOLOGY

Sharon F. Freedman, MD, professor of ophthalmology and pediatric ophthalmology and strabismus division chief and her colleagues have had a productive year with continued clinical research in a variety of areas—childhood glaucoma diagnosis and treatment, retinal and optic nerve imaging using optical coherence tomography (OCT), and retinopathy of prematurity (ROP) research.
Tono-Pen Comparison
Along with former Duke pediatric fellows Allison Umfress, MD, Tanya Glaser, MD and Pimpiroon Ploysangam, MD, Freedman studied the use of a newly-approved device (iCare IC200) for measuring the eye pressure of children either sitting up (in clinic) or in the supine position (for babies lying down or children supine under anesthesia). The authors compared the iCare IC200 device against the commonly used Tono-Pen for assessing eye pressure under anesthesia in the operating room, and against the gold standard Goldmann applanation device in the clinic. This work validated the new iCare IC200 device as an important supplemental tool for eye pressure assessment in the operating room for children requiring examination under anesthesia to evaluate the control of their glaucoma. This study was published in the Journal of the American Association for Pediatric Ophthalmology and Strabismus in November 2021.

Risk for Childhood Glaucoma: 10 Year Follow Up
Freedman was the first and corresponding author on a publication in JAMA Ophthalmology in December 2020 that reported the incidence of glaucoma and glaucoma suspect diagnoses among children 10 years following participation in the NIH-sponsored Infant Aphakia Treatment Study. This pivotal study randomized infants having a unilateral cataract removed in the first six months.
Duke ROPtool May Advance ROP Diagnosis
Continuing their long-standing interest in the way that blood vessels change their thickness and tortuosity in the retina of prematurely born infants with ROP, corresponding author S. Grace Prakalapakorn, MD, MPH, Freedman and co-authors used a semi-automated computer program (ROPtool) developed by the group, to quantitatively compare the blood vessel changes over time between infants eventually requiring treatment for severe ROP versus those who never needed treatment. Published in the Journal of the American Association for Pediatric Ophthalmology and Strabismus in February 2021, the study documented clinically relevant quantifiable differences in the retinal blood vessel characteristics of these two groups of eyes. This work shows potential to advance our ability to identify eyes at highest risk of developing severe ROP before they need treatment by utilizing computer-based quantification.
THE GLAUCOMA GENE OPTINEURIN PROTECTS AGAINST VIRAL INFECTION IN THE EYE AND BRAIN

Duke glaucoma specialist Henry Tseng, MD, PhD discovered an important novel function for a gene called Optineurin, through a collaboration with an interdisciplinary team of virologists at the University of Illinois Chicago over many years. This gene is associated with glaucoma, amyotrophic lateral sclerosis (ALS) and may play a role in other neurodegenerative diseases such as Alzheimer’s, Parkinson’s, and Huntington’s diseases. This exciting work was reported in two recently published papers in Nature Communications and Journal of Immunology.
Tseng, associate professor of ophthalmology, and his colleagues found that optineurin plays a critical part in neuroinflammatory response and host defense against simple ubiquitous viruses such as Herpes Simplex Viruses (HSV-1 and HSV-2) Specifically, optineurin confers protection for brain cells in the eye and the brain. This function is critical to prevent neurodegenerative changes triggered by viral infections.
These experiments were made possible using a novel transgenic mouse generated in Dr. Tseng’s laboratory at the Duke Eye Center. In this mouse, the optineurin gene was genetically removed, and thus allowed the research team to investigate how brain cells respond to viral infections without optineurin function.

HSV-1 infections typically cause limited mouth cold sores and superficial corneal eye infections. However, in Dr. Tseng’s transgenic knockout mice without the optineurin gene, herpesvirus rapidly spread from the surface of the eye into corneal nerves and finally into the brain. Surprisingly, this neuroinvasive infection resulted in diffuse brain degeneration and animal death within weeks. In sharp contrast, without HSV-1 infection, these transgenic mice can live up to 2 years.
The team also delineated a molecular mechanism and showed that a potential chemical compound can limit neurodegeneration. Further research work is needed to determine its clinical utility.
Because HSV-1 infection is ubiquitous and present in 60-80% of adults, findings in this work may be relevant to many patients with glaucoma and other neurodegenerative diseases. By improving our understanding of how genetic mutations lead to brain cell loss, this work offers potential novel strategies for developing new treatments for glaucoma, ALS, Alzheimer’s disease, and other neurodegenerative diseases.
A DOCTOR WHO WEARS TWO HATS (OR SCRUB CAPS): AESTHETIC AND FUNCTIONAL

Julie A. Woodward, MD, professor of ophthalmology, and chief of the oculofacial and reconstructive surgery division continues to be a leader in the field.
Woodward and colleagues compared water absorption of FDA-approved hyaluronic acid fillers, published in Dermatologic Surgery in September 2021.
The goal of this study was to provide long-term insight into an improved, tailored facial rejuvenation approach and to understand sequelae that could affect preoperative surgical planning.
The findings show hyaluronic acid facial fillers absorb water and delayed tissue swelling after injection. It may take months or even years for the swelling to become evident in the lower or upper eyelids, resulting in a displeasing aesthetic outcome that may require dissolving the filler with hyaluronidase. This publication is the first to attempt to identify fillers that may carry increased in vitro risk of delayed edema, although the authors stress all HA fillers carry this potential.
There were three types of fillers where the water absorption was low, thus making these good options for under eye filler. Fillers with more water absorption may be beneficial for enhancement of the lips. The results inform us about in vivo conditions and provide guidance for filler selection.
In addition to this important research, Woodward took part in the first ever clinical trial for under eye filler for FDA approval. She was invited to share the data with plastic surgeons, facial plastic surgeons, dermatologists, and physician extenders during a medical aesthetics training course in San Diego in January 2022.
Woodward is involved in research for both aesthetic and functional medicine. Her aesthetic research is primarily focused on patient safety through study of vascular anatomy, ability to dissolve facial fillers and rheologic measurements of extrusion forces that lead to improved techniques for new injectors to ensure safety when treating patients. She also conducts research for medical and surgical therapies to treat benign essential blepharospasm, a functionally blinding condition.
Woodward serves on two medical boards, the Aesthetics Industry Association and the Benign Essential Blepharospasm Research Foundation (BEBRF). She enjoys speaking directly to the patients through lectures organized by the BEBRF.
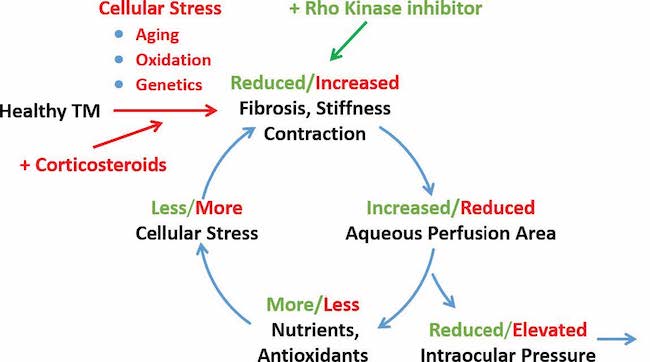
STUDY SHOWS NETARSUDIL EFFECTIVE IN TREATING STEROID INDUCED GLAUCOMA

Researchers at Duke Eye Center have identified that netarsudil is particularly effective at treating steroid induced glaucoma. Results of the study were published in eLife in March 2021.
Glaucoma is a leading cause of blindness throughout the world, which can be caused by some medications. Glucocorticoids, a type of steroid are widely used for treating common eye conditions and diseases, often causing ocular hypertension—increased pressure in the eyes that can threaten vision. Eye pressure increase from steroids occurs in up to one-third of the general population and over 90% of people with glaucoma. In this study, Daniel W. Stamer, PhD (corresponding author) and Pratap Challa, MD (co-author) report that an FDA-approved drug called netarsudil, a rho-kinase inhibitor, decreased glucocorticoid-induced ocular hypertension in patients whose intraocular pressures were poorly controlled by standard medications. Using a mouse model of glucocorticoid-induced ocular hypertension, the team then looked at the processes behind this positive effect of netarsudil, and saw that the drug both reduced and prevented the root cause for elevated intraocular pressure.
These important findings suggest the need for a randomized prospective clinical study to see whether netarsudil is superior to first-line anti-glaucoma drugs in lowering steroid induced ocular hypertension. This study shows promise that netarsudil could become a mainstream treatment for patients at risk for steroid-induced ocular hypertension.

Trainee Awards
The 2021 Heed Fellowship was awarded to:


Oleg Alekseev, MD, PhD received the Research to Prevent Blindness (RPB) Small Grant Award through the Duke Eye Center Unrestricted Institutional Grant. This grant supports his research to develop novel therapeutics for retinitis pigmentosa. He is pursuing this work under the mentorship of Vadim Arshavsky, PhD.
Jordan Deaner, MD received the 2021 Ronald G. Michels Foundation Fellowship Award.

Priya Gupta, MD received the Retina Research Foundation/Joseph M. and Eula C. Lawrence Travel Grant for her project titled “A Complex Retinal Dystrophy-obesity Phenotype is Associated with Compound Heterozygous Loss-of-function TUB Gene Mutations” under the mentorship of Alessandro Iannaccone, MD, MS, FARVO. She was awarded a Clinical Research Fellowship Award through the Foundation Fighting Blindness to fund her research during her Inherited Retinal Dystrophy fellowship at Mass Eye and Ear.
Honors and Awards

Tammy Hsu, MD received an award for Top 10 Presentations for her work under the mentorship of Julie Woodward, MD, on the interactions of hyaluronidase with hyaluronic acid-based fillers at the 2021 Cosmetic Surgery Forum.

Grant Justin, MD received the 2021 Achievement Award for his contributions made to the American Academy of Ophthlamology, its scientific and educational programs and to ophthalmology. He received the 2021 VitreoRetinal Surgery Foundation (VRSF) Award for his project “Evaluating the Retinal Structure and Microvasculature in Mild and Moderate Traumatic Brain Injury using Multimodal Retinal Imaging“ under the mentorship of Sharon Fekrat, MD, FACS, FASRS and Dilraj Grewal, MD.

Michael Quist, MD was honored as The American Academy of Ophthalmology (AAO) 2020 Copeland Fellow.

Cason Robbins, MD received the Retina Research Foundation/Joseph M. and Eula C. Lawrence Travel Grant for his project titled “Analyzing the Retinal and Choroidal Vasculature and Structure in Cognitively Healthy Individuals at Higher Genetic Risk for Alzheimer’s Disease using a Convolutional Neural Network” under the mentorship of Sharon Fekrat, MD, FACS, FASRS and Dilraj Grewal, MD. He received the departmental Research to Prevent Blindness Small Grant Award, Duke Eye Center for his project titled “Correlating retinal and choroidal microvascular parameters with volumetric MRI in Alzheimer’s disease and mild cognitive impairment” under the mentorship of Sharon Fekrat, MD, FACS, FASRS and Dilraj Grewal, MD.

Nita Valikodath, MD received the VitreoRetinal Surgery Foundation (VRSF) Award for her project, “Screening for Pediatric Retinal Diseases Using Artificial Intelligence and Wide-field Fundus Imaging” under the mentorship of Lejla Vajzovic, MD.

C. Ellis Wisely MD, MBA received the departmental Research to Prevent Blindness Small Grant Award for his project titled “Correlation of aqueous humor and serum protein concentrations of amyloid, tau, neurofilament light chain, and alpha-synuclein with neurodegenerative disease” under the mentorship of Sharon Fekrat, MD, FACS, FASRS.

Steph Zhang, MD received the American Society of Cataract and Refractive Surgery (ASCRS) 2021 Resident Excellence Award.

Yuxi Zheng, MD received the Top Poster Award for her work under the mentorship of Sharon Fekrat, MD, FACS, FASRS titled “Vitreomacular Status in Eyes with CRVO: Complete Vitreomacular Separation in Eyes with CRVO Predicts Treatment Burden and Clinical Outcomes” during the 2021 Women in Ophthalmology Summer Symposium.


Medical Student Awards

Dennis Akrobetu received the Gerhard Zinser Memorial Travel Grant for his project titled “Assessment of Retinal Microvascular Alterations in Individuals with Amnestic and Non-amnestic Mild Cognitive Impairment Using Optical Coherence Tomography Angiography” under the mentorship of Sharon Fekrat, MD, FACS, FASRS and Dilraj Grewal, MD.

Jennifer Chang received the Knights Templar Eye Foundation Travel Grant for her project titled “Cost Comparison of Reusable versus Disposable Equipment for Retinopathy of Prematurity Screening Rounds” under the mentorship of S. Grace Prakalapakorn, MD, MPH and Sharon F. Freedman, MD with additional support from Dr. Evan Myers, MD, MPH.

Praruj Pant received the 2021 VitreoRetinal Surgery Foundation (VRSF) Award for his project “Longitudinal assessment of choroidal vascularity index, subfoveal choroidal thickness, and central subfield thickness in treatment-naïve eyes with cystoid macular edema due to branch retinal vein occlusion compared to unaffected fellow eyes” under the mentorship of Sharon Fekrat, MD, FACS, FASRS. He received 3rd place at the NCSEPS 2021 Poster Competition for his collaborative project with trainees Xinxin Zhang, MD and Yuxi Zheng, MD titled “Vitreomacular status in eyes with CRVO” under the mentorship of Sharon Fekrat, MD, FACS, FASRS.

Camille Robinson received the Knights Templar Eye Foundation Travel Grant for her project titled “Glaucoma Knowledge and Disease Severity in a Veteran Population with Poor Adherence.” Her mentors on the project are Jullia Rosdahl, MD, PhD and Kelly Muir, MD, as well as Duke glaucoma fellow Andrew Williams, MD.

Kai Seely was awarded the “Retina Research Foundation/Joseph M. and Eula C. Lawrence Travel Grant” for ARVO 2021.

Resident Grand Rounds
- April 19, 2022
- May 24, 2022
- September 15, 2022
- October 18, 2022
- November 18, 2022
- December 2, 2022
Virtual Education Series
- March 14, 2022
- April 4, 2022
- May 16, 2022
- June 21, 2022
- September 19, 2022
- October 27, 2022
- November 14, 2022
- December 12, 2022
Duke Cornea Fellows Program *NEW* :
April 1, 2022
Controversies in Cornea and Cataract Surgery Conference
April 2, 2022
8th Annual Duke Fellow Advanced Vitreous Surgery Course (fAVS)
May 20-21, 2022
Duke Ophthalmology Trainee Scientific Session: A Presentation of Trainee Scientific Discoveries
June 3, 2022
34th Annual Glaucoma Symposium
September 10, 2022
Duke Glaucoma Fellows Program
September 29, 2022 in Chicago at AAO
22nd Annual Duke Advanced Vitreous Surgery Course (AVS)
March 24-25, 2023
Advances in Pediatric Retina Conference (APR)
Held every other year, date to be determined for 2023
Distinguished Lectures
The Stephen and Frances Foster Distinguished Lecture
April 11, 2022
Stephen Pflugfelder, MD
Professor and James and Margaret Elkins Chairman in Ophthalmology
Baylor College of Medicine
Science Professor Lecture
April 14, 2022
Adriana Di Polo, PhD, ARVO
Professor in Neuroscience and Ophthalmology
University of Montreal
Joseph M. Bryan Lecture
April 21, 2022
Gregory S. Hageman, PhD, FARVO
John A Moran Presidential Professor
Department of Ophthalmology and Visual Sciences
University of Utah School of Medicine
Director, Moran Center for Translational Medicine, Salt Lake City, Utah
The Annual Diversity and Inclusion Lecture Series
June 23, 2022
Eve J. Higginbotham SM, MD, ML
Vice Dean for Penn Medicine Office of Inclusion and Diversity
Senior Fellow, Leonard Davis Institute for Health Economics
Professor of Ophthalmology
Perelman School of Medicine
University of Pennsylvania
Gordon K. Klintworth, MD, PhD Distinguished Lecture
June 30, 2022
Robert F. Mullins, MS, PhD
Martin Carver Chair in Ocular Cell Biology
Professor of Ophthalmology and Visual Sciences
Carver College of Medicine
University of Iowa
The Dastgheib Pioneer Award in Ocular Innovation Lecture
September 30, 2022
José-Alain Sahel, MD
Distinguished Professor and Chairman
Department of Ophthalmology
University of Pittsburgh School of Medicine
Exceptional Class Professor at Sorbonne Université, Paris
The Eye and Ear Foundation Endowed Chair
Inaugural Mittra Family Foundation Lecture
October 27, 2022
Daniel F. Martin, MD
Chairman, Cole Eye Institute
Cleveland Clinic
Joseph M. Bryan Lecture
November 17, 2022
Rando Allikmets, PhD
Acquavella Professor, Department of Ophthalmology
Research Director, Harkness Eye Institute Columbia University
Visit dukeeyecenter.duke.edu for more information.
Duke Eye on Education
Duke Eye Center has remained committed for decades to providing valuable educational opportunities to support the professional development of faculty, trainees, and ophthalmic colleagues.
The last 2 years have presented challenges which required a transition to a collaborative but safe virtual platform for educational events offered by Duke Eye Center. Through successful navigation, this opportunity allowed the CME team to realize the benefits provided by this new virtual stage.
Duke Eye Center has experienced continued success with the CME program. Virtual platforms have enabled an increase in the number of events offered and allowed expanded access to domestic and international attendance.
Not bound by the physical limits of a venue, an increase in space and opportunities for a larger number of generous exhibitors and sponsors have maximized educational offerings.
While continuing to offer the flexibility that accompany virtual meetings, there is an eagerness to resume invaluable face-to-face learning and networking provided by in-person conferences. In the coming year, hybrid meetings will be offered that will allow attendees to choose participation, either in person or by a virtual platform.

Educational events planned for 2022 include distinguished lectures by world-renowned ophthalmology researchers, clinicians and clinician scientists, robust sub-specialty focused conferences and wet labs, internationally focused events, monthly lecture series, and interactive grand rounds.
“While the last two years have been daunting, the continuing education program at Duke Eye Center has flourished. I am optimistic for the future and have high hopes to see our colleagues again in-person while also offering a virtual option to attend,” said Lejla Vajzovic, MD, Associate Professor of Ophthalmology and Director of Continuing Medical Education.