We believe that the emergence of new ideas from different perspectives catalyzes innovation and success. In support of our mission, we view diversity, defined as encompassing all aspects of human differences, as a fundamental pillar to fostering an inclusive working and learning environment, where all individuals feel respected, are treated fairly, provided work-life balance, and an opportunity to excel in their respective fields.
EDI Spotlight: Omar Mohiuddin, OTR/L, MS, MPH, CLVT
Over the years as an occupational therapist, Omar Mohiuddin, OTR/L, MS, MPH, CLVT, came to realize that many accessibility issues often go unaddressed, even in spaces originally designed with older adults and persons with visual impairment in mind. That realization fueled his passion for accessibility and drives his devotion to improving the day-to-day lives of persons with blindness and low vision.
Enyedi Discusses Sexual Harassment in Ophthalmology Study on Mend the Gap Podcast
Laura Enyedi, MD led a discussion on the Sexual Harassment in Ophthalmology study on a recent episode of the Mend the Gap podcast.
Herndon Discusses the Importance of Mentors in Career Development
Professor of Ophthalmology Leon Herndon, MD was featured in a recent Healio article discussing the importance of mentorship in ophthalmology.
Use of Service Animals in Healthcare Settings
For centuries, dogs have assisted people with disabilities to perform routine daily activities. Formalizing canine assistance began in 1916 when the German Shepherd Dog Society trained dogs to support German veterans blinded during World War I. Responding to requests from blind Americans, in 1929 US dog breeder and philanthropist Dorothy Harrison Eustis founded The Seeing Eye, the first US program to train guide dogs. For decades, with their rigid, U-shaped harnesses, Seeing Eye dogs were America’s quintessential service animals.
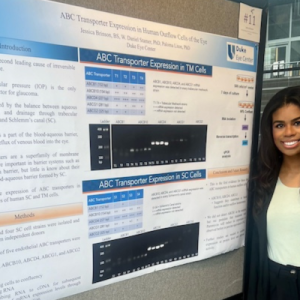
Duke OPSD Summer Academy Student Receives 1st Place at Howard Research Symposium
Jessica Brinson received the 1st place award at the Orthopedic Women of Howard Research Symposium. Brinson, a medical student at Howard University College of Medicine, participated in the Duke Office of Physician-Scientist Development Summer Academy. During the program, she worked with mentors Paloma Liton, PhD and Daniel Stamer, PhD to investigate the role of ABC transporters in glaucoma.
Duke Eye Resident Accepted to ASRS Underrepresented in Retina Mentorship Program
Duke Eye Center is thrilled to announce that Duke PGY-3 resident, Richard Morgan, MD, PhD, has been accepted into the prestigious American Society of Retina Specialists’ (ASRS) Underrepresented in Retina Mentorship Program. This groundbreaking initiative is designed to cultivate diversity within the field by providing invaluable mentorship opportunities to residents from underrepresented backgrounds. Through this program, mentees like Dr.
Toth Featured on Mend the Gap Podcast
Cynthia Toth, MD shared stories from her career as a female surgeon in ophthalmology during the latest Mend the Gap podcast by Healio. Laura Enyedi, MD co-hosted the podcast.
Statement on Violence in Israel and Gaza
Dear Friends and Colleagues,
Over the last several days we have been shocked, saddened, and somewhat paralyzed with a sense of helplessness as we have watched the violence unfold and escalate in Israel and Gaza. Many of us are experiencing a complex set of emotions including fear, anxiety, and anger. For the faculty, trainees, and staff who have loved ones or ties to the region, our thoughts are with you, we support you, and raise our voices for peace along your side.
Ask the OEDI: Hispanic, Latino, Latina, Latinx - Which is Best?
A variety of terms are used to describe people who come from, or have family roots coming from, countries in Latin America and the Caribbean. In the United States, two terms are most frequently used, sometimes interchangeably: Hispanic, and some variation of Latino, Latina, or Latinx.
Annual DEI Lecture Featuring Tamara Fountain, MD
Duke Eye Center had the honor of hosting the Annual Equity, Diversity and Inclusion Lecture on July 18, featuring guest speaker, Tamara Fountain, MD, 125th President of the American Academy of Ophthalmology. Fountain's lecture, "Headwinds and Headway - Striving for Best Outcomes in All Our Patients" can be viewed at the link below.